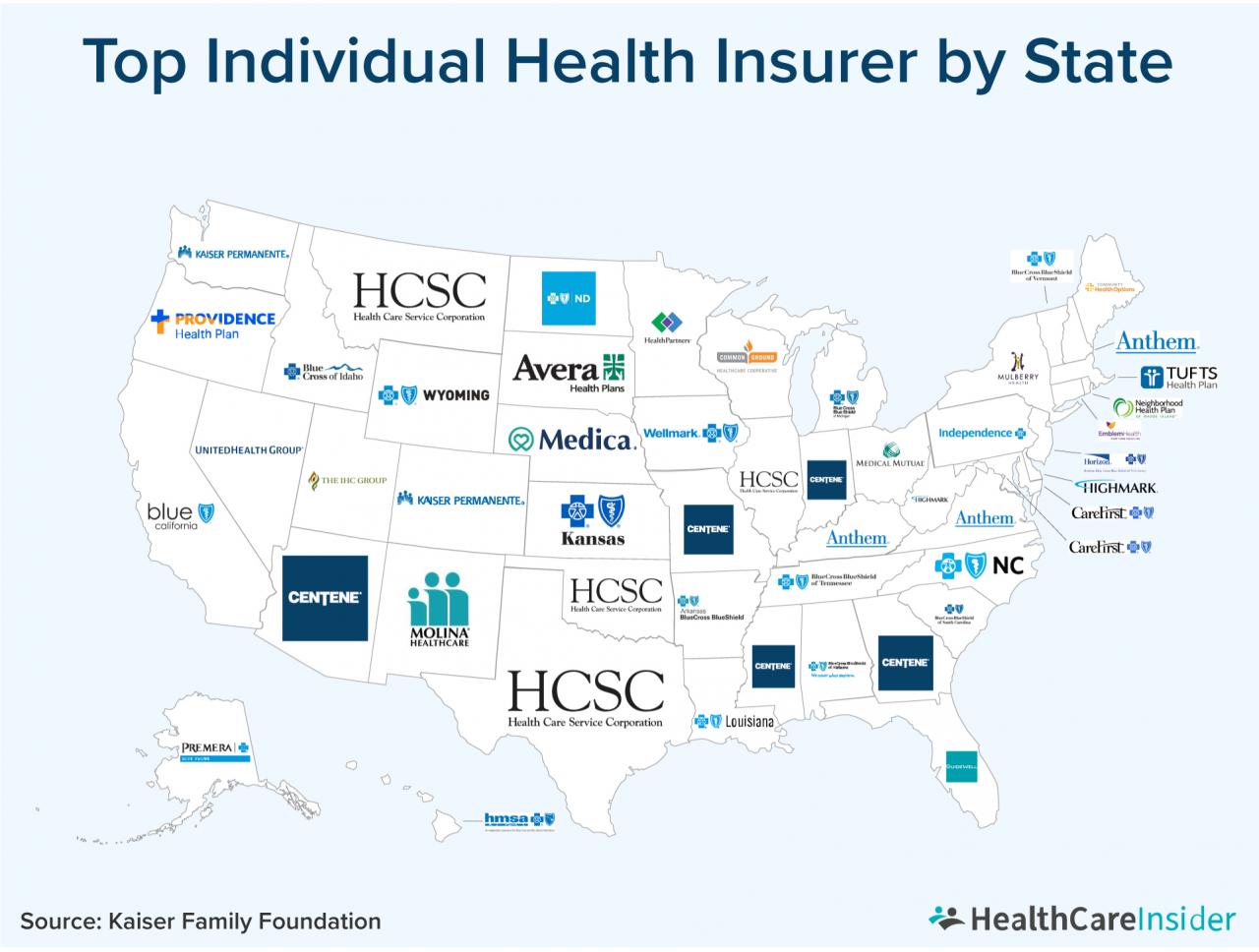
- Defining Commercial Health Insurance
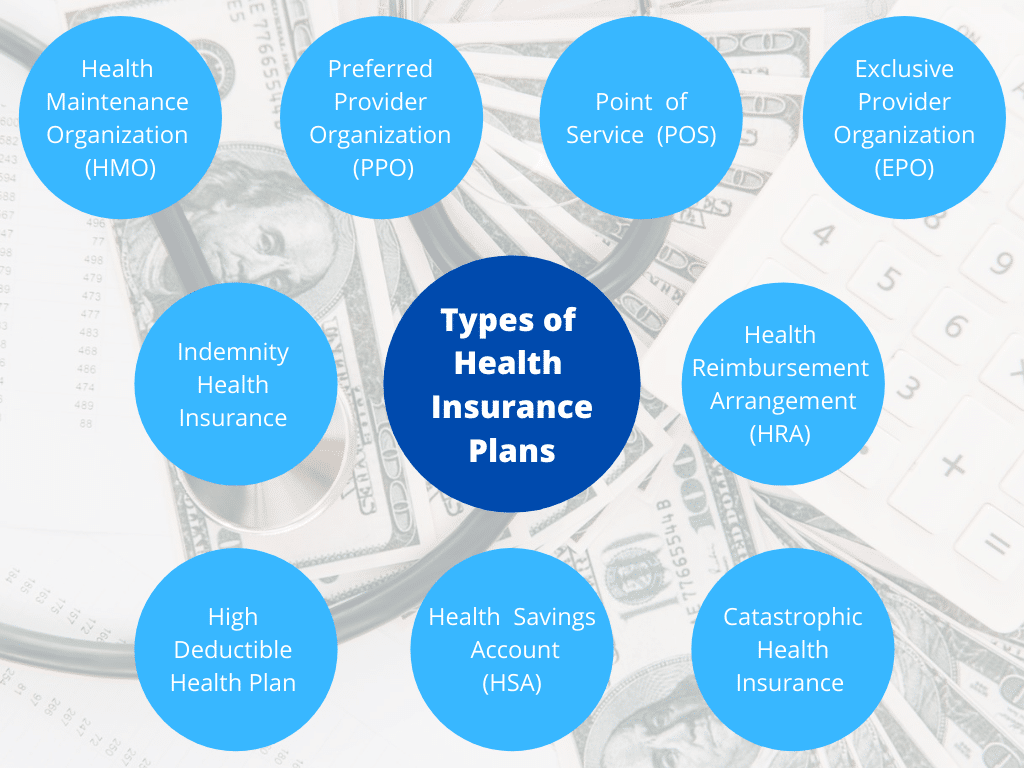
- Types of Commercial Health Insurance Plans
- Key Components of a Commercial Health Insurance Policy
- Benefits and Advantages of Commercial Health Insurance
- Considerations When Choosing a Commercial Health Insurance Plan
- The Role of Health Insurance Brokers and Agents
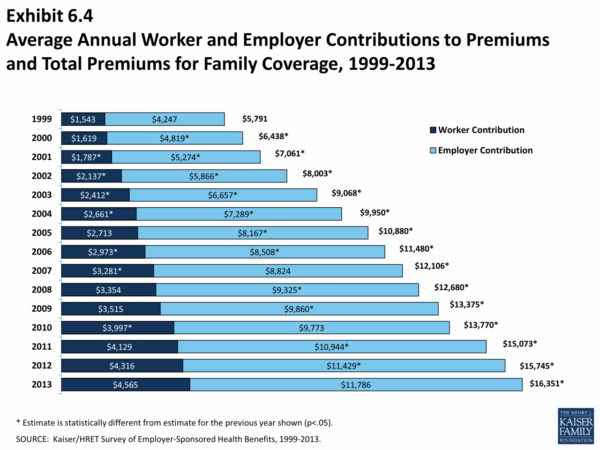
- Understanding Health Insurance Premiums and Costs
- The Importance of Open Enrollment Periods
- The Impact of Health Reform on Commercial Health Insurance
- Understanding Common Terms and Concepts: What Is A Commercial Health Insurance
- Final Review
- Popular Questions
What is a commercial health insurance – What is commercial health insurance? It’s a type of insurance policy that individuals and families purchase to protect themselves from the financial burden of unexpected medical expenses. Unlike government-funded programs like Medicare or Medicaid, commercial health insurance is offered by private companies and provides coverage for a wide range of medical services, from routine checkups to hospitalization and surgery.
The purpose of commercial health insurance is to provide financial security and peace of mind, knowing that you have a safety net in place should you face a health crisis. This guide will delve into the intricacies of commercial health insurance, exploring its different types, key components, benefits, and considerations when choosing a plan.
Defining Commercial Health Insurance
Commercial health insurance is a type of insurance that helps individuals and families pay for healthcare expenses. It is offered by private companies, unlike government-sponsored programs like Medicare and Medicaid.
Characteristics of Commercial Health Insurance
Commercial health insurance is characterized by several key features that differentiate it from other types of insurance.
- Private Coverage: It is provided by private companies, unlike government-sponsored programs.
- Premium Payments: Policyholders pay premiums to the insurance company in exchange for coverage.
- Coverage Options: Commercial health insurance plans offer various coverage options, including individual, family, and group plans.
- Network Restrictions: Most commercial health insurance plans have networks of healthcare providers, which are doctors, hospitals, and other healthcare professionals that the insurer has contracted with.
- Deductibles and Co-pays: Policyholders typically have to pay a deductible, which is a fixed amount they must pay out-of-pocket before the insurance company begins to cover costs. They may also have to pay co-pays, which are fixed amounts they pay for each healthcare service, such as a doctor’s visit or prescription.
- Benefit Limits: Commercial health insurance plans may have limits on the amount of coverage they provide. For example, a plan may have a lifetime maximum on the amount of benefits it will pay out.
Types of Commercial Health Insurance Plans
Commercial health insurance plans offer various options to cater to different needs and preferences. Understanding the different types of plans available can help you choose the best fit for your individual circumstances.
Health Maintenance Organization (HMO)
HMOs are known for their cost-effectiveness and emphasis on preventative care. They operate under a network model, requiring members to choose a primary care physician (PCP) within the network.
The PCP acts as a gatekeeper, referring members to specialists within the network only when necessary.
- Coverage: HMOs typically cover preventive care, routine checkups, and basic medical services. They may have limited coverage for out-of-network services, often requiring higher out-of-pocket costs.
- Benefits: HMOs often offer lower premiums compared to other plans. They may also provide access to wellness programs and disease management services.
- Example: A young, healthy individual with a limited budget might find an HMO plan suitable. They can benefit from lower premiums and access to preventive care services.
Preferred Provider Organization (PPO)
PPOs offer more flexibility than HMOs, allowing members to seek care from both in-network and out-of-network providers.
While in-network services are typically covered at a lower cost, out-of-network services are covered at a higher cost with a higher copay or coinsurance.
- Coverage: PPOs generally offer broader coverage compared to HMOs, including out-of-network services.
- Benefits: PPOs provide more flexibility in choosing providers and offer wider network access. However, premiums may be higher than HMOs.
- Example: An individual with a chronic condition who prefers a specific specialist outside the network might find a PPO plan more suitable. They can access out-of-network care with some coverage, although at a higher cost.
Point of Service (POS)
POS plans combine elements of both HMOs and PPOs. They offer network-based care but allow for out-of-network access with higher costs.
POS plans require members to choose a PCP within the network but allow them to seek care outside the network with a referral from their PCP.
- Coverage: POS plans provide coverage for both in-network and out-of-network services, with higher costs for out-of-network care.
- Benefits: POS plans offer some flexibility in provider choice and network access while maintaining lower premiums compared to PPOs.
- Example: A family with a mix of health needs might find a POS plan suitable. They can access in-network care at lower costs while having the option to seek out-of-network care for specific needs.
High Deductible Health Plan (HDHP)
HDHPs are characterized by high deductibles and low premiums.
Members pay a higher deductible before the insurance coverage kicks in.
- Coverage: HDHPs typically cover essential health benefits but have high deductibles. They may offer lower premiums compared to other plans.
- Benefits: HDHPs often allow individuals to open a Health Savings Account (HSA), which offers tax advantages for saving for healthcare expenses.
- Example: Individuals with good health and a lower risk of frequent healthcare utilization might find an HDHP suitable. They can save on premiums and potentially benefit from the HSA.
Key Components of a Commercial Health Insurance Policy
A commercial health insurance policy is more than just a piece of paper; it’s a contract outlining the financial protection you’ll receive for healthcare expenses. Understanding its key components is crucial for making informed decisions about your coverage and maximizing its benefits.
Deductibles
Deductibles represent the amount you must pay out-of-pocket before your insurance coverage kicks in. Imagine it as a threshold you need to cross before your insurer starts sharing the cost of your healthcare.
For example, if your deductible is $1,000, you’ll need to pay the first $1,000 of your medical expenses yourself. Once you’ve met that threshold, your insurance will start covering the remaining costs according to your plan’s terms.
Higher deductibles often translate to lower monthly premiums, but you’ll bear a larger financial burden upfront. Lower deductibles mean higher premiums but lower out-of-pocket costs when you need care.
Copayments
Copayments are fixed amounts you pay for specific healthcare services, such as doctor’s visits or prescriptions. They are typically a set dollar amount, regardless of the total cost of the service.
For instance, you might pay a $20 copayment for a doctor’s visit or a $10 copayment for a generic prescription.
Copayments help manage healthcare costs by encouraging patients to be more conscious of their healthcare spending.
Coinsurance, What is a commercial health insurance
Coinsurance is a percentage of the healthcare costs you share with your insurance company after you’ve met your deductible.
For example, if your coinsurance is 20%, you’ll pay 20% of the cost of a covered medical service after meeting your deductible, and your insurance company will cover the remaining 80%.
Coinsurance helps spread the cost of healthcare between you and your insurer, particularly for larger medical expenses.
Out-of-Pocket Maximum
The out-of-pocket maximum represents the most you’ll have to pay for covered healthcare expenses in a given year. Once you reach this limit, your insurance company will cover 100% of the remaining costs for covered services.
For example, if your out-of-pocket maximum is $5,000, even if your medical expenses exceed that amount, you won’t pay more than $5,000 in a year.
Out-of-pocket maximums provide a safety net against unexpected high medical costs, offering peace of mind knowing there’s a limit to your financial responsibility.
Coverage Limitations and Exclusions
It’s essential to understand what your insurance policy covers and what it doesn’t. Policies typically have limitations and exclusions, which specify certain services, treatments, or conditions that aren’t covered.
For example, some policies may exclude coverage for pre-existing conditions, experimental treatments, or cosmetic procedures.
Carefully review your policy documents to understand these limitations and exclusions to avoid unexpected costs.
Benefits and Advantages of Commercial Health Insurance
Commercial health insurance offers a range of benefits that can significantly improve your financial well-being and access to quality healthcare. By providing financial protection against unexpected medical expenses and facilitating access to a wide range of healthcare services, commercial health insurance plays a crucial role in safeguarding your health and peace of mind.
Financial Protection Against Unexpected Medical Expenses
Medical emergencies and unexpected illnesses can be financially devastating. Commercial health insurance acts as a financial safety net, mitigating the financial burden associated with these events. The insurance policy covers a significant portion of your medical expenses, including hospitalization, surgery, and medication costs. This financial protection helps prevent you from facing substantial out-of-pocket expenses, ensuring you can focus on your recovery without worrying about the financial implications.
Enhanced Access to Quality Healthcare Services
Commercial health insurance provides access to a wide network of healthcare providers, including hospitals, clinics, and specialists. This network ensures you have access to quality healthcare services, regardless of your location. The insurance policy also covers preventive care services, such as regular checkups and screenings, which can help detect health issues early and improve your overall well-being.
Considerations When Choosing a Commercial Health Insurance Plan
Choosing the right commercial health insurance plan can be a daunting task, as numerous factors come into play. It’s crucial to carefully evaluate your individual needs and preferences before making a decision. This section explores key considerations to guide you in selecting a plan that best suits your circumstances.
Understanding Your Healthcare Needs
It’s essential to assess your healthcare needs and identify the level of coverage you require. Factors to consider include:
- Your Age and Health Status: Younger individuals with good health may opt for a lower-cost plan with less coverage, while older individuals or those with pre-existing conditions might prefer a plan with comprehensive benefits.
- Your Family Size and Composition: Families with children or dependents may require plans with broader coverage, including pediatric care and maternity benefits.
- Your Lifestyle and Healthcare Habits: If you have a high-risk lifestyle, such as engaging in extreme sports or having specific dietary needs, you might require a plan with specialized coverage.
- Your Prescription Drug Needs: Consider your current and potential future prescription drug requirements, as some plans have limited formularies or higher co-pays for certain medications.
Comparing Premium Costs and Coverage
Commercial health insurance plans vary significantly in terms of premium costs and coverage levels. It’s crucial to compare different options and determine the best value for your money.
- Premium Costs: Premium costs are the monthly payments you make for your health insurance coverage. Factors influencing premiums include age, health status, location, and the plan’s coverage level.
- Deductibles: The deductible is the amount you pay out-of-pocket before your insurance coverage kicks in. Higher deductibles generally translate to lower premiums, while lower deductibles lead to higher premiums.
- Co-pays and Co-insurance: Co-pays are fixed amounts you pay for specific services, while co-insurance represents a percentage of the cost you share with your insurer. These factors influence the out-of-pocket expenses you incur for healthcare services.
- Coverage Limits: Each plan has coverage limits, such as maximum annual out-of-pocket expenses or lifetime limits on certain services. It’s crucial to understand these limitations to avoid unexpected costs.
Evaluating Network Size and Provider Availability
The network size and provider availability are crucial factors to consider, as they determine your access to healthcare services.
- Network Size: A broader network offers access to a wider range of healthcare providers, including doctors, hospitals, and specialists. However, plans with smaller networks may have lower premiums.
- Provider Availability: Ensure that your preferred doctors and healthcare facilities are included in the plan’s network. If you have specific healthcare needs, such as a specialist or a particular hospital, check if they are part of the network.
Analyzing Plan Features and Benefits
Commercial health insurance plans offer various features and benefits beyond basic coverage. It’s essential to compare these features and determine which ones align with your needs.
- Preventive Care Coverage: Most plans cover preventive services, such as annual checkups and screenings, at no cost. This can help you stay healthy and avoid costly medical treatments in the long run.
- Mental Health and Substance Abuse Coverage: Some plans offer comprehensive mental health and substance abuse coverage, including therapy sessions and medication.
- Telehealth and Virtual Care: Telehealth services provide access to healthcare professionals remotely, offering convenience and affordability for certain medical consultations.
- Wellness Programs: Some plans offer wellness programs that encourage healthy habits and provide incentives for healthy behaviors, such as fitness activities or healthy eating plans.
The Role of Health Insurance Brokers and Agents
Navigating the complex world of health insurance can be overwhelming, especially with the wide array of plans and options available. This is where health insurance brokers and agents play a crucial role. They act as intermediaries between individuals and insurance companies, providing valuable assistance in the selection process.
Services Provided by Brokers and Agents
Brokers and agents offer a range of services to help individuals find the right health insurance plan. These services are designed to simplify the process and ensure that individuals make informed decisions.
- Guidance and Advice: Brokers and agents possess in-depth knowledge of the insurance market and various plan options. They can provide personalized guidance based on individual needs, health status, and budget. They can explain the intricacies of different plans, including coverage details, deductibles, co-pays, and out-of-pocket expenses.
- Plan Comparisons: Brokers and agents can compare plans from multiple insurance companies, highlighting key differences and benefits. This allows individuals to make side-by-side comparisons and identify the plan that best meets their requirements. They can also help individuals understand the trade-offs involved in different plans, such as higher premiums for broader coverage.
- Enrollment Assistance: Once an individual selects a plan, brokers and agents can assist with the enrollment process. They can help with paperwork, answer questions, and ensure a smooth transition to the new plan.
- Ongoing Support: Brokers and agents can provide ongoing support even after enrollment. They can answer questions, help with claims, and assist with any changes to the plan. This ongoing support ensures individuals have a reliable resource throughout their insurance journey.
Finding Reputable Brokers and Agents
Finding a reputable and knowledgeable broker or agent is essential for a positive experience. Here are some tips for identifying qualified professionals:
- Check Credentials and Licensing: Ensure that brokers and agents are licensed and certified in your state. This indicates they have met the necessary requirements and are authorized to sell insurance.
- Seek Recommendations: Ask friends, family, or colleagues for recommendations. Their experiences can provide valuable insights into the quality of service provided by specific brokers or agents.
- Research Online: Use online resources such as the National Association of Health Underwriters (NAHU) or the Council of Insurance Agents & Brokers (CIAB) to find reputable brokers and agents in your area.
- Schedule Consultations: Contact multiple brokers or agents to schedule consultations. This allows you to ask questions, discuss your needs, and gauge their knowledge and expertise.
Understanding Health Insurance Premiums and Costs
Your health insurance premium is the monthly amount you pay to maintain your coverage. It’s like a subscription fee that ensures you have access to medical care when you need it.
How Health Insurance Premiums Are Calculated
Insurance companies use a complex formula to determine your premium, taking into account various factors. They analyze your individual risk profile to estimate how much they might need to pay for your healthcare needs in the future.
Factors Influencing Premium Costs
- Age: Younger individuals generally have lower premiums than older individuals because they tend to have fewer health issues. As you age, the risk of needing medical care increases, leading to higher premiums.
- Health Status: If you have pre-existing health conditions, your premium might be higher because you’re considered a higher risk to the insurance company.
- Location: Premiums can vary depending on where you live. Factors like the cost of living, availability of healthcare providers, and the prevalence of certain health conditions in your area can influence premium costs.
- Tobacco Use: Smokers typically pay higher premiums because smoking increases the risk of health problems.
- Plan Type: Different types of health insurance plans have varying premium costs. Plans with higher deductibles and copayments usually have lower premiums, while plans with lower deductibles and copayments typically have higher premiums.
- Family Size: Premiums for family plans are generally higher than premiums for individual plans, reflecting the increased potential for healthcare expenses.
Components of a Health Insurance Premium
| Component | Description |
|---|---|
| Base Premium | This is the core cost of your health insurance policy, determined by your age, location, and plan type. |
| Risk Adjustment | This factor reflects your individual health status, such as pre-existing conditions or lifestyle choices. |
| Administrative Costs | These costs cover the insurance company’s expenses for running the business, such as marketing, claims processing, and customer service. |
| Profit Margin | Insurance companies need to make a profit to stay in business. This component represents the company’s desired profit margin. |
| Taxes | Depending on your location, your premium may include taxes. |
The Importance of Open Enrollment Periods
Open enrollment periods are crucial for commercial health insurance, as they represent the designated time frame during which individuals and businesses can enroll in, change, or cancel their health insurance plans without facing penalties. This period offers a chance to evaluate existing coverage, explore new options, and make informed decisions about health insurance needs.
Missing Open Enrollment Periods
Missing an open enrollment period can have significant implications, potentially leading to penalties or limitations on plan selection. If you miss the open enrollment period, you may only be able to enroll in a new plan if you experience a qualifying life event, such as getting married, having a baby, or losing your job. These events allow you to enroll in a new plan outside the open enrollment period, but your options may be limited.
It’s important to note that even if you have a qualifying life event, you may not be able to switch to a different plan during the special enrollment period. You may be limited to enrolling in a plan that is offered by your employer or through the Marketplace.
Key Dates and Deadlines
Open enrollment periods vary depending on the type of health insurance plan. For individual health insurance plans offered through the Marketplace, the open enrollment period typically runs from November 1st to January 15th. For employer-sponsored health insurance plans, the open enrollment period is usually set by the employer and may vary in length.
- Individual Health Insurance Plans (Marketplace): The open enrollment period for individual health insurance plans offered through the Marketplace typically runs from November 1st to January 15th.
- Employer-Sponsored Health Insurance Plans: Open enrollment periods for employer-sponsored health insurance plans are usually set by the employer and may vary in length.
It is essential to be aware of the specific open enrollment dates and deadlines for your health insurance plan. Contact your insurance provider or employer to confirm the exact dates for your plan.
The Impact of Health Reform on Commercial Health Insurance

The Affordable Care Act (ACA), also known as Obamacare, has significantly reshaped the landscape of commercial health insurance in the United States. Its implementation brought about numerous changes, impacting coverage, affordability, and accessibility of healthcare for millions of Americans. This section explores the key effects of this landmark legislation on commercial health insurance.
Changes in Coverage
The ACA introduced several provisions aimed at expanding coverage and improving healthcare access. These include:
- Essential Health Benefits: The ACA mandates that all health insurance plans, including commercial plans, must cover a set of essential health benefits, such as preventive care, hospitalization, and prescription drugs. This ensures that individuals have access to a comprehensive range of healthcare services.
- Pre-existing Conditions: The ACA prohibits insurance companies from denying coverage or charging higher premiums based on pre-existing conditions. This has been a significant benefit for individuals with chronic illnesses, who previously faced challenges in obtaining affordable health insurance.
- Dependent Coverage: The ACA allows young adults to remain on their parents’ health insurance plans until the age of 26, expanding coverage for a critical age group.
- Individual Mandate: The ACA originally required most individuals to have health insurance or face a penalty. This provision aimed to encourage more people to enroll in health insurance, thereby expanding the risk pool and potentially lowering premiums for all. However, the individual mandate penalty was eliminated in 2019.
Changes in Affordability
The ACA has also had a notable impact on the affordability of commercial health insurance:
- Premium Tax Credits: The ACA provides premium tax credits to eligible individuals and families, helping them afford health insurance. These credits are based on income and are available through the Health Insurance Marketplace.
- Cost-Sharing Reductions: The ACA also offers cost-sharing reductions to help lower out-of-pocket costs for individuals with lower incomes. These reductions can help reduce the burden of deductibles, copayments, and coinsurance.
- Medicaid Expansion: The ACA expanded Medicaid eligibility, providing health insurance coverage to millions of low-income Americans. This expansion has significantly reduced the number of uninsured individuals and has contributed to increased affordability of healthcare.
Changes in Accessibility
The ACA has also improved the accessibility of commercial health insurance:
- Health Insurance Marketplace: The ACA created the Health Insurance Marketplace, a platform where individuals can compare and purchase health insurance plans from different insurers. This platform has streamlined the process of finding and enrolling in health insurance, making it more accessible to a wider population.
- Navigators and Enrollers: The ACA also funded the training and deployment of navigators and enrollers to assist individuals in navigating the health insurance marketplace and enrolling in plans. This support has been crucial in helping individuals understand their options and make informed choices.
Future Trends and Implications
The impact of the ACA on commercial health insurance continues to evolve, and several trends are worth noting:
- Continued Evolution of the Marketplace: The Health Insurance Marketplace is expected to continue to evolve, with new features and improvements being implemented to enhance its functionality and accessibility.
- Focus on Value-Based Care: The healthcare industry is shifting towards value-based care models, where providers are incentivized to deliver high-quality care at a lower cost. This trend is likely to impact commercial health insurance plans, with insurers seeking to partner with providers who demonstrate value in their care delivery.
- Increased Use of Technology: The use of technology in healthcare is expected to continue to grow, leading to the development of innovative tools and services for managing health insurance and accessing care.
Potential Future Implications
The ACA has undoubtedly brought about significant changes in commercial health insurance, and its long-term implications are still unfolding. Some potential future implications include:
- Changes in Insurance Premiums: The ACA’s impact on insurance premiums is a complex issue. While the individual mandate and premium tax credits have helped stabilize premiums, the cost of healthcare continues to rise, potentially leading to future premium increases.
- Changes in Plan Design: As the healthcare landscape evolves, commercial health insurance plans may need to adapt their design to meet the changing needs of consumers. This could involve the introduction of new benefits, the adjustment of coverage levels, or the development of innovative plan options.
- Increased Competition: The ACA has fostered greater competition in the health insurance market, with new insurers entering the marketplace and existing insurers expanding their offerings. This increased competition could lead to lower premiums and improved plan choices for consumers.
Understanding Common Terms and Concepts: What Is A Commercial Health Insurance
Navigating the world of commercial health insurance can feel overwhelming, especially with the abundance of unfamiliar terms and concepts. Understanding these terms is crucial for making informed decisions about your health insurance plan. This section will define some key terms that are commonly used in the context of commercial health insurance.
Key Terms in Commercial Health Insurance
Understanding the key terms used in commercial health insurance plans is essential for navigating your coverage and making informed decisions about your health care. Here are some common terms you should be familiar with:
- Deductible: The amount of money you must pay out-of-pocket for covered health care expenses before your health insurance plan starts paying its share. For example, if your deductible is $1,000, you would need to pay the first $1,000 of covered medical expenses yourself before your insurance kicks in.
- Co-pay: A fixed amount you pay for a specific medical service, such as a doctor’s visit or prescription drug, at the time of service. For example, you might have a $20 co-pay for a doctor’s visit and a $10 co-pay for a generic prescription.
- Co-insurance: A percentage of the cost of covered health care services that you are responsible for paying after you have met your deductible. For example, if your co-insurance is 20%, you would pay 20% of the cost of covered medical services after you have met your deductible.
- Premium: The monthly payment you make to your health insurance company to maintain your coverage. Premiums can vary depending on factors such as your age, location, health status, and the type of plan you choose.
- Out-of-pocket maximum: The maximum amount of money you are responsible for paying for covered health care expenses in a given year. Once you reach this limit, your insurance plan will cover 100% of the remaining eligible costs.
- Pre-existing conditions: Medical conditions that you had before you enrolled in a health insurance plan. Some health insurance plans may exclude coverage for pre-existing conditions, or they may charge higher premiums for individuals with pre-existing conditions.
- Coordination of benefits (COB): A process used to determine which health insurance plan is primary and which is secondary when an individual has coverage under multiple plans. This is common for individuals who are covered under both their employer’s plan and their spouse’s plan. The primary plan is typically the one that pays first, while the secondary plan pays any remaining costs.
- Out-of-network coverage: The benefits you receive for health care services provided by providers who are not part of your insurance plan’s network. Out-of-network coverage is typically less comprehensive and may require you to pay a higher percentage of the costs.
- Network: A group of healthcare providers, such as doctors, hospitals, and pharmacies, that have contracted with your health insurance company to provide services at a discounted rate.
- Formulary: A list of prescription drugs that are covered by your health insurance plan. Your insurance plan may require you to use generic drugs when they are available, and it may not cover certain brand-name drugs.
- Benefit period: The period of time during which your health insurance coverage is in effect. Most health insurance plans have a benefit period of one year.
- Open enrollment period: A specific time of year when you can enroll in a health insurance plan or change your existing plan without facing penalties.
Final Review
Understanding commercial health insurance is crucial for making informed decisions about your healthcare. By carefully considering your individual needs, comparing plan options, and engaging with knowledgeable brokers or agents, you can find a plan that best suits your circumstances and provides you with the financial protection and access to quality healthcare you deserve.
Popular Questions
How does commercial health insurance work?
Commercial health insurance operates by pooling premiums from a large group of individuals or families to create a fund that can be used to cover medical expenses. When you need healthcare, you file a claim with your insurance company, which will then pay a portion of your medical bills, depending on your plan’s coverage and your deductible and co-pay amounts.
What are the different types of commercial health insurance plans?
There are several types of commercial health insurance plans, each with its own coverage structure and network of providers. Some common types include HMOs, PPOs, POSs, and HDHPs. The best plan for you will depend on your individual needs and preferences.
How much does commercial health insurance cost?
The cost of commercial health insurance varies depending on factors such as your age, health status, location, and the type of plan you choose. Premiums can be paid monthly or annually.
What is the open enrollment period for commercial health insurance?
The open enrollment period for commercial health insurance is a specific time frame during which you can enroll in or change your health insurance plan without facing penalties. This period typically occurs once a year.