- Age Limits and Eligibility
- Dependency Status
- Financial Independence
- Marriage and Other Life Events: How Long Can My Son Stay On My Health Insurance
- Health Insurance Marketplace Options
- Employer-Sponsored Coverage
- State-Specific Programs
- Open Enrollment Periods
- Potential Consequences of Delayed Enrollment
- Closure
- FAQs
How long can my son stay on my health insurance? This question often arises as parents navigate the complex world of health insurance and plan for their children’s future. Understanding the factors that determine eligibility, such as age limits, dependency status, and financial independence, is crucial for ensuring continuous coverage. Navigating the intricacies of health insurance can be daunting, but by understanding the rules and options, parents can make informed decisions about their children’s healthcare.
This guide explores the key factors that influence how long a child can remain on a parent’s health insurance plan. We’ll delve into age limits, dependency status, financial independence, and the impact of life events like marriage. We’ll also examine alternative options such as the health insurance marketplace and employer-sponsored plans. By understanding these factors, parents can gain clarity on their children’s coverage and make informed decisions about their healthcare needs.
Age Limits and Eligibility
It’s important to understand the age limits for children remaining on a parent’s health insurance. These limits are influenced by a combination of federal regulations and state laws.
Age Limits for Children on Parent’s Health Insurance
Federal law, through the Affordable Care Act (ACA), requires health insurance plans to allow children to stay on their parents’ plan until they turn 26. This applies to both individual and employer-sponsored plans.
However, state laws can extend this coverage even further. Some states allow children to stay on their parents’ plan beyond age 26, particularly for specific circumstances, such as attending school or being disabled.
Examples of Different Insurance Plans and Age Limits
Here are some examples of how different insurance plans handle age limits for children:
* Individual Health Insurance Plans: Most individual health insurance plans follow the federal mandate of allowing children to stay on their parents’ plan until age 26.
* Employer-Sponsored Health Insurance Plans: Employer-sponsored plans are also required to follow the federal mandate of allowing children to stay on their parents’ plan until age 26.
* State-Specific Health Insurance Plans: Some states have their own laws that extend coverage beyond the federal mandate. For example, California allows children to stay on their parents’ plan until age 26 even if they are no longer a student or dependent.
Important Note: It’s crucial to check with your specific insurance provider to confirm the exact age limits and eligibility requirements for your plan.
Dependency Status
Your child’s dependency status is a crucial factor in determining how long they can remain on your health insurance plan. It refers to whether your child meets the legal criteria to be considered dependent for insurance purposes.
The concept of dependency status ensures that children are covered under their parents’ health insurance plans until they reach a certain age or achieve a specific level of independence.
Situations Affecting Dependency Status
Several factors can influence a child’s dependency status.
- Age: Most health insurance plans consider children dependent until they turn 26. However, some plans may have different age limits, so it’s essential to review your policy details.
- Full-time Student Status: If your child is a full-time student, they may be considered dependent even if they’ve turned 26, but this depends on the specific insurance plan.
- Disability: If your child is disabled and unable to support themselves, they may qualify for coverage under your plan even after turning 26. This is usually determined by the insurance company’s definition of disability.
- Marital Status: Generally, marriage terminates dependency status, meaning your child would no longer be eligible for coverage under your plan. However, some plans may have exceptions, such as if the marriage is considered invalid or short-lived.
Financial Independence
A child’s financial independence is a significant factor in determining their eligibility for parental health insurance. If a child is considered financially independent, they may no longer be eligible to be covered under their parents’ plan.
The primary factor in determining financial independence is the child’s ability to support themselves financially. This means that they have a stable income and are not reliant on their parents for financial assistance.
Income and Financial Support
Income is a key indicator of financial independence. If a child has a steady income from a job or other sources, they are more likely to be considered financially independent. However, income alone may not be enough. The amount of income, the source of the income, and the child’s financial responsibilities will all be considered.
The amount of financial support that a child receives from their parents is also important. If a child is still receiving significant financial support from their parents, they may not be considered financially independent, even if they have a job. This support could include paying for housing, food, transportation, or other expenses.
Examples of Financial Independence
There are many scenarios where a child might be considered financially independent. Here are some examples:
- A child who is employed full-time and has a stable income that covers all of their living expenses.
- A child who is self-employed and has a successful business that generates enough income to support themselves.
- A child who has a significant amount of savings and investments that provide them with enough income to live independently.
- A child who has received a large inheritance or other windfall that allows them to be financially independent.
Marriage and Other Life Events: How Long Can My Son Stay On My Health Insurance

Getting married or experiencing other significant life events can impact your son’s ability to remain on your health insurance. These events often affect dependency status and insurance eligibility, so it’s essential to understand how they can influence coverage.
Marriage
Generally, when your son gets married, he is no longer considered a dependent for health insurance purposes. This is because marriage typically signifies financial independence, and your son’s spouse’s employer may offer health insurance as a benefit. However, there are some exceptions to this rule.
Military Service
If your son enlists in the military, he may be eligible to remain on your health insurance plan, even if he’s married. The Military Health System (MHS) provides healthcare services to active-duty military personnel and their families. However, the specific rules for dependents’ coverage vary depending on the branch of service and the individual’s circumstances.
Starting a Family, How long can my son stay on my health insurance
Having children doesn’t automatically disqualify your son from remaining on your health insurance plan. However, if he is no longer financially dependent on you, he may need to obtain his own coverage. The rules regarding dependent coverage can vary depending on the insurance plan, so it’s essential to consult with your insurance provider for specific details.
Health Insurance Marketplace Options
The Health Insurance Marketplace, also known as the Affordable Care Act (ACA) Marketplace, offers a variety of health insurance plans for individuals and families. These plans are offered by private insurance companies and are regulated by the federal government.
Marketplace Plan Types
The Marketplace offers four main types of health insurance plans:
- Bronze plans: Bronze plans have the lowest monthly premiums but also the highest out-of-pocket costs. They cover about 60% of the average person’s healthcare costs.
- Silver plans: Silver plans have moderate monthly premiums and out-of-pocket costs. They cover about 70% of the average person’s healthcare costs.
- Gold plans: Gold plans have higher monthly premiums but lower out-of-pocket costs. They cover about 80% of the average person’s healthcare costs.
- Platinum plans: Platinum plans have the highest monthly premiums but the lowest out-of-pocket costs. They cover about 90% of the average person’s healthcare costs.
Cost and Benefits Comparison
| Plan Type | Monthly Premium | Deductible | Co-insurance | Out-of-Pocket Maximum |
|---|---|---|---|---|
| Bronze | Lowest | Highest | Highest | Highest |
| Silver | Moderate | Moderate | Moderate | Moderate |
| Gold | Highest | Lowest | Lowest | Lowest |
| Platinum | Highest | Lowest | Lowest | Lowest |
Eligibility for Subsidized Coverage
Individuals and families may be eligible for subsidies to help pay for their health insurance premiums through the Marketplace. These subsidies are based on income and family size. For example, a family of four with an annual income of $60,000 may be eligible for a subsidy to help pay for their health insurance premiums.
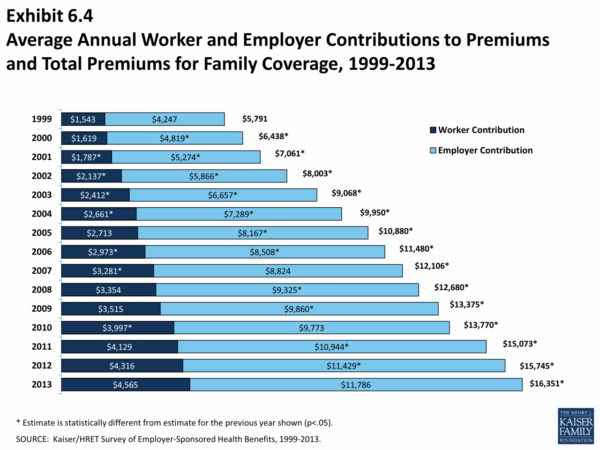
Employer-Sponsored Coverage
Your son may be able to obtain health insurance through your employer’s plan. This is often a great option for families, as employer-sponsored plans typically offer affordable coverage and comprehensive benefits.
Employer-sponsored plans can be a valuable resource for families, providing affordable and comprehensive coverage for children. However, eligibility requirements and limitations vary depending on the employer’s plan and the child’s age.
Eligibility Requirements
To be eligible for coverage under your employer’s plan, your son must meet certain requirements. These requirements typically include:
* Age: Most plans cover children until they reach a certain age, often 26.
* Dependency Status: Your son must be considered a dependent under your employer’s plan. This usually means he is unmarried, under 26, and financially dependent on you.
* Residency: Your son may need to reside in the same state as you.
Limitations
While employer-sponsored plans offer many benefits, they may also have limitations:
* Waiting Periods: There may be a waiting period before your son can enroll in the plan.
* Coverage Limits: Some plans may have coverage limits for certain services or procedures.
* Cost-Sharing: You may be responsible for copayments, coinsurance, or deductibles for your son’s healthcare services.
Scenarios Where Employer-Sponsored Coverage Might Be Suitable
Here are some examples of scenarios where employer-sponsored coverage might be a suitable option:
* Young Children: Employer-sponsored plans are often a good choice for covering young children, as they typically offer comprehensive benefits and affordable premiums.
* College Students: If your son is a full-time student under the age of 26, he may be eligible for coverage under your employer’s plan, even if he is not financially dependent on you.
* Families with Limited Income: Employer-sponsored plans can be a more affordable option than purchasing individual health insurance, especially for families with limited income.
State-Specific Programs
Many states have their own programs designed to provide health insurance options for children, even if they are not eligible for Medicaid or CHIP. These programs often have different eligibility criteria and benefits, so it’s important to research the options available in your specific state.
State-Specific Children’s Health Insurance Programs
These programs are designed to provide health insurance coverage to children who are not eligible for Medicaid. They often have income-based eligibility requirements and may offer a range of benefits, including coverage for doctor visits, hospital stays, prescription drugs, and dental care.
- Example: In California, the Healthy Families program provides health insurance to children from low-income families. The program’s eligibility requirements are based on family income and size, and it offers comprehensive health coverage.
- Example: The Children’s Health Insurance Program (CHIP) in Texas, known as STAR Kids, offers health insurance to children from low-income families. The program covers a wide range of health services, including preventive care, immunizations, and mental health services.
State-Specific Programs for Uninsured Children
Some states offer programs specifically for children who are uninsured and do not qualify for Medicaid or CHIP. These programs may provide subsidies or other financial assistance to help families afford health insurance.
- Example: The New York State of Health marketplace offers a range of health insurance plans for children, including plans with subsidies for low-income families.
- Example: In Massachusetts, the Commonwealth Care program offers health insurance plans for children, including plans with subsidies for low-income families.
Impact on Eligibility for Parental Insurance
State-specific programs can impact a child’s eligibility to remain on a parent’s insurance in a few ways.
- Eligibility Requirements: Some programs may have eligibility requirements that conflict with the rules for remaining on a parent’s insurance. For example, a child may be eligible for a state-specific program based on income, but may not be eligible to remain on a parent’s insurance if the parent’s income is above a certain threshold.
- Cost Considerations: If a child is eligible for a state-specific program, it may be more affordable than remaining on a parent’s insurance. In this case, the family may choose to enroll the child in the state program.
- Age Limits: State-specific programs may have age limits that differ from the age limits for remaining on a parent’s insurance. This means that a child may become eligible for a state program after they are no longer eligible to remain on a parent’s insurance.
Open Enrollment Periods
Open enrollment periods are specific times of the year when you can make changes to your health insurance plan, like switching to a different plan or adding or removing coverage for your child. Understanding these periods is crucial, as they affect when you can make adjustments to your health insurance coverage.
Timing of Open Enrollment Periods
Open enrollment periods for individual health insurance plans, which are purchased directly from insurance companies, typically occur once a year, usually in the fall. This period allows individuals to compare different plans and choose the one that best suits their needs and budget.
Open enrollment periods for individual health insurance plans usually run from November 1st to January 15th.
However, there are some exceptions. For example, if you experience a qualifying life event, such as getting married, having a baby, or losing your job, you may be eligible for a special enrollment period to make changes outside of the regular open enrollment period.
Examples of Open Enrollment Period Use
Here are some scenarios where your child might need to enroll in a new plan during open enrollment:
- Your child turns 26 and is no longer eligible to be covered under your plan. You will need to enroll them in a new plan during the next open enrollment period.
- Your child’s health insurance needs change. For example, if your child develops a chronic condition, you may need to switch to a plan with better coverage for that condition.
- You move to a new state. Your child’s current plan may not be available in your new state, so you will need to enroll them in a new plan during the next open enrollment period.
Potential Consequences of Delayed Enrollment

Delaying enrollment in health insurance can have significant consequences, potentially leading to coverage gaps, higher costs, and even denied claims. Understanding the risks associated with delayed enrollment is crucial to ensure continuous and affordable healthcare access.
Coverage Gaps
Delaying enrollment can create a coverage gap, leaving you without health insurance during a crucial period. This can be particularly problematic if you experience an unexpected health issue or require medical treatment during this gap.
For instance, if you delay enrollment for a few months and then get into an accident requiring hospitalization, you might face substantial out-of-pocket expenses for medical bills.
Higher Costs
In many cases, delaying enrollment can result in higher premiums. This is because insurance companies often offer lower rates to individuals who enroll during open enrollment periods or within a specified timeframe.
For example, if you miss the open enrollment period and enroll later, you might be subject to a higher premium or face a penalty.
Denied Claims
Delaying enrollment can also lead to denied claims, especially if you develop a pre-existing condition during the coverage gap. Insurance companies might deny coverage for conditions that arise before you enroll, even if you eventually secure coverage.
For example, if you delay enrollment and develop a pre-existing condition like diabetes, your insurance company might refuse to cover treatment costs related to this condition.
Closure

Ensuring your child’s health insurance coverage requires careful planning and understanding of the various factors involved. From age limits and dependency status to financial independence and life events, several elements influence how long a child can stay on a parent’s plan. By staying informed and exploring available options, parents can navigate the complexities of health insurance and make informed choices to secure their children’s healthcare.
FAQs
What happens if my child turns 26 and is still a full-time student?
Even if your child is a full-time student, they will typically lose coverage at age 26. However, some states have exceptions, so it’s important to check your state’s specific rules.
Can my child stay on my health insurance if they are married?
Generally, marriage terminates a child’s eligibility for coverage under a parent’s plan. However, some plans might have exceptions, so it’s essential to review your policy details.
What if my child is disabled?
If your child has a disability, they may be eligible to remain on your plan beyond age 26. Specific rules vary, so consult your insurance provider or refer to your state’s guidelines.
Is there a way to keep my child on my health insurance after they turn 26?
While it’s generally not possible to keep your child on your plan after they turn 26, some exceptions might apply, such as disability or certain state-specific programs. Contact your insurance provider for details.