Will health insurance cover oral surgery? This is a common question for many individuals, especially when faced with the prospect of needing a procedure like wisdom teeth removal or dental implants. The answer, however, is not always straightforward. Coverage for oral surgery depends on various factors, including the type of procedure, your insurance plan, and your overall health status. Understanding the nuances of oral surgery coverage can help you navigate the process effectively and minimize potential out-of-pocket costs.
This guide explores the intricacies of oral surgery coverage, offering insights into the types of procedures typically covered, factors influencing coverage, potential out-of-pocket expenses, and strategies for finding the right insurance plan. Whether you’re seeking information about common procedures like tooth extractions or less frequent procedures like bone grafts, this guide provides a comprehensive overview of what to expect when it comes to oral surgery and insurance.
Understanding Oral Surgery Coverage
Understanding what your health insurance covers when it comes to oral surgery is crucial for planning and budgeting. It can help you avoid unexpected expenses and ensure you receive the necessary care.
Types of Oral Surgeries Covered
Most health insurance plans cover a range of oral surgeries that are considered medically necessary. These surgeries are typically performed to address issues affecting your overall health, not just your teeth.
- Extractions: Removing teeth due to decay, infection, or crowding.
- Implants: Replacing missing teeth with artificial roots and crowns.
- Bone Grafting: Adding bone to the jaw to support implants or prepare for other procedures.
- Wisdom Teeth Removal: Removing impacted wisdom teeth that can cause pain, infection, or damage to other teeth.
- Cleft Palate Repair: Surgery to correct a birth defect that affects the roof of the mouth.
- Tumor Removal: Removing cancerous or non-cancerous growths in the mouth.
Factors Influencing Coverage
Several factors determine whether your health insurance will cover a specific oral surgery.
- Medical Necessity: The primary factor is whether the surgery is considered medically necessary to address a health condition.
- Pre-authorization: Many insurance plans require pre-authorization for oral surgery, which involves getting approval from your insurer before the procedure.
- Plan Coverage: Different insurance plans have varying levels of coverage for oral surgery. Some plans may have specific limits on the types of procedures covered or the amount they will pay.
- Network Provider: Your insurance plan may have a network of preferred providers. Out-of-network providers may have different coverage levels.
Dental Plans and Oral Surgery Coverage
Dental plans, such as dental insurance or dental HMOs, typically offer coverage for oral surgery.
- Dental Insurance: Provides coverage for a range of dental services, including oral surgery.
- Dental HMOs: Offer a more limited network of providers and typically have lower premiums than traditional dental insurance.
Coverage Comparison
Different insurance plans may have different coverage levels for oral surgery.
- Co-pays: Some plans may require you to pay a co-pay for each visit or procedure.
- Deductibles: You may have to pay a deductible before your insurance starts covering the costs.
- Co-insurance: You may be responsible for a percentage of the costs after your deductible is met.
- Maximum Benefit: Insurance plans may have a maximum amount they will pay for dental services in a year.
Factors Influencing Coverage

The factors determining whether your health insurance covers oral surgery are numerous and interconnected. It’s crucial to understand these factors to determine what your plan covers and what out-of-pocket expenses you might incur.
Pre-Authorization
Pre-authorization is a crucial aspect of oral surgery coverage. It’s a process where your insurance provider reviews the proposed procedure and determines if it’s medically necessary and covered under your plan.
Pre-authorization is a pre-approval process by your insurance provider before a procedure is performed. It’s typically required for major oral surgeries like dental implants or jaw surgery.
- Purpose: To ensure the procedure is medically necessary and within the scope of your insurance plan.
- Process: You or your dentist will submit a request for pre-authorization to your insurance company. This request will include details about the procedure, your medical history, and the reason for the surgery.
- Importance: Pre-authorization can help avoid unexpected costs and ensure that your surgery is covered. If your insurance provider denies pre-authorization, you can appeal the decision or consider alternative treatment options.
Patient’s Health Condition
Your health condition plays a significant role in determining whether your insurance plan will cover oral surgery.
- Pre-existing Conditions: If you have a pre-existing health condition that impacts your oral health, your insurance company might cover the surgery as part of your overall medical care. For example, if you have diabetes, your insurance may cover oral surgery to prevent complications from uncontrolled blood sugar levels.
- Medical Necessity: Your insurance provider will assess whether the surgery is medically necessary to address your health condition. If the surgery is deemed elective, meaning it’s not essential for your health, it might not be covered.
Limitations and Exclusions
Every insurance plan has its limitations and exclusions. Understanding these limitations is crucial to avoid unexpected costs.
- Cosmetic Procedures: Most insurance plans don’t cover cosmetic oral surgery, such as teeth whitening or veneers, unless they are medically necessary to address a health condition.
- Waiting Periods: Some insurance plans have waiting periods before they cover certain dental procedures, including oral surgery. This means you may have to wait a specific period before your coverage kicks in.
- Annual Limits: Many insurance plans have annual limits on dental coverage. If you exceed this limit, you might have to pay out-of-pocket for any additional procedures, including oral surgery.
Out-of-Pocket Costs
Oral surgery can be a significant financial investment, and understanding the potential out-of-pocket costs is crucial for budgeting and planning. This section will explore the typical out-of-pocket costs associated with oral surgery, including deductibles, copayments, and other expenses.
Deductibles and Copayments
Deductibles and copayments are common components of health insurance plans that contribute to out-of-pocket costs.
- Deductibles: A deductible is the amount you must pay out-of-pocket before your insurance starts covering the costs of your oral surgery. Deductibles vary depending on your insurance plan and can range from a few hundred dollars to several thousand dollars.
- Copayments: A copayment is a fixed amount you pay for each service, such as a consultation or surgery. Copayments are typically lower than deductibles and are often applied to specific services, like office visits or procedures.
Common Out-of-Pocket Expenses
The following table Artikels common out-of-pocket expenses for various oral surgeries.
| Oral Surgery | Deductible | Copayment | Other Expenses |
|---|---|---|---|
| Wisdom Tooth Extraction | $500 – $2,000 | $25 – $50 per visit | Anesthesia, medications, post-surgery care |
| Implants | $1,000 – $3,000 | $50 – $100 per visit | Crowns, bone grafting, lab fees |
| Bone Grafting | $500 – $1,500 | $25 – $50 per visit | Materials, anesthesia |
Minimizing Out-of-Pocket Costs
There are several strategies you can use to minimize out-of-pocket costs for oral surgery.
- Negotiate with Your Dentist: You can negotiate with your dentist for a lower fee or payment plan.
- Shop Around for Insurance: Compare different health insurance plans to find one with lower deductibles and copayments for oral surgery.
- Consider a Health Savings Account (HSA): An HSA allows you to set aside pre-tax money to pay for medical expenses, including oral surgery.
- Ask About Financing Options: Some dental offices offer financing options, such as payment plans or loans.
Finding the Right Coverage
Navigating the world of health insurance can be a complex task, especially when it comes to understanding oral surgery coverage. This section will guide you through the process of determining if your current plan covers oral surgery and how to select a plan with comprehensive coverage.
Reviewing Your Current Plan
The first step is to thoroughly examine your existing health insurance policy. Most plans provide a summary of benefits, which should clearly Artikel the coverage for dental procedures. Look for specific language related to oral surgery, including:
- Covered procedures: This list will detail the types of oral surgeries your plan covers, such as wisdom tooth extraction, dental implants, or jaw surgery.
- Benefit limits: Your plan may have annual or lifetime limits on the amount of coverage for oral surgery. Understanding these limits will help you budget for any potential out-of-pocket expenses.
- Co-pays and deductibles: These are the fixed amounts you’ll pay for each covered service and the minimum amount you need to pay before your insurance kicks in, respectively. These can significantly impact your overall cost.
- Network restrictions: Some plans require you to use specific dentists or oral surgeons within their network to receive full coverage. Make sure you understand these restrictions and choose a provider within your network if necessary.
Selecting a Plan with Comprehensive Coverage
If your current plan doesn’t offer sufficient oral surgery coverage, or you’re looking for a new plan, here are some key considerations:
- Dental coverage: Many health insurance plans offer separate dental coverage, which may be included in your existing plan or available as an add-on. Look for plans that provide comprehensive dental coverage, including oral surgery.
- Network options: Consider plans with wide networks that include dentists and oral surgeons you trust or who are conveniently located.
- Premium costs: Compare premium costs for different plans with similar coverage levels. Keep in mind that plans with more comprehensive coverage often come with higher premiums.
- Out-of-pocket expenses: Evaluate the potential out-of-pocket costs, including deductibles, co-pays, and coinsurance. Plans with lower out-of-pocket expenses can save you money in the long run, especially for significant procedures.
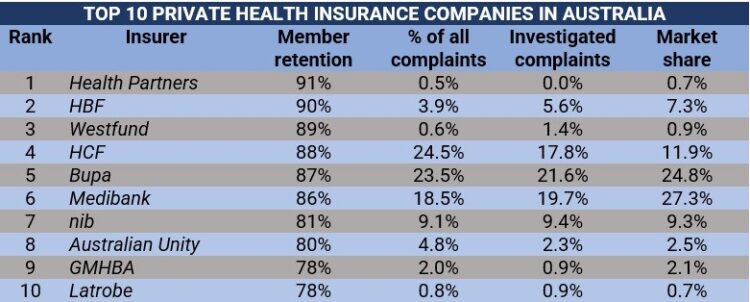
Comparing Insurance Plans
To effectively compare plans, use the following tips:
- Use online comparison tools: Many websites allow you to compare plans side-by-side, including their coverage details and costs.
- Contact insurance providers directly: Speak with insurance representatives to clarify any unclear details or ask specific questions about their oral surgery coverage.
- Read policy documents carefully: Don’t just rely on summaries; review the full policy documents to understand the fine print and potential limitations.
Key Features Comparison
Here’s a table comparing key features of different insurance plans regarding oral surgery coverage:
| Plan Name | Annual Limit | Deductible | Co-pay | Network Size |
|---|---|---|---|---|
| Plan A | $1,000 | $500 | $25 | Small |
| Plan B | $2,000 | $250 | $50 | Medium |
| Plan C | $5,000 | $0 | $75 | Large |
Commonly Covered Procedures
While every insurance plan is different, there are some common oral surgeries that are typically covered. These procedures are generally considered medically necessary to address dental problems that affect your overall health.
Extractions
Extractions are procedures to remove teeth. Extractions are usually covered when the tooth is severely damaged, decayed, or infected, and cannot be saved with other treatments.
- Simple Extraction: This involves removing a tooth that is visible above the gum line. It is often covered when the tooth is severely decayed or damaged.
- Surgical Extraction: This involves removing a tooth that is impacted (trapped below the gum line or bone), broken, or otherwise difficult to remove. It is often covered when the tooth is causing pain, infection, or other complications.
For example, if a tooth is severely decayed and causing pain or infection, your insurance may cover the cost of extraction.
Implants
Dental implants are artificial tooth roots that are surgically placed into the jawbone. They provide a stable foundation for crowns, bridges, or dentures. Insurance coverage for implants is usually limited to situations where they are necessary to restore function and prevent further dental problems.
- Single Tooth Implant: This involves placing a single implant to replace a missing tooth. It is often covered when the tooth loss is due to injury, disease, or decay.
- Multiple Tooth Implants: This involves placing multiple implants to replace several missing teeth. It is often covered when the tooth loss is due to advanced periodontal disease or other conditions.
For example, if you have lost a tooth due to an accident and it is causing problems with your bite or chewing, your insurance may cover the cost of a single tooth implant.
Bone Grafting, Will health insurance cover oral surgery
Bone grafting is a procedure that involves adding bone to the jawbone to improve the quality or quantity of bone. This is often necessary before placing dental implants or other procedures. Insurance coverage for bone grafting is usually limited to situations where it is medically necessary.
- Sinus Lift: This involves adding bone to the jawbone in the area of the sinuses. It is often necessary to support dental implants in the upper jaw.
- Ridge Augmentation: This involves adding bone to the jawbone to increase the width or height of the ridge. It is often necessary to support dental implants or other procedures.
For example, if you have lost a tooth due to periodontal disease and the bone in your jaw has deteriorated, your insurance may cover the cost of a bone graft to support a dental implant.
Wisdom Tooth Removal
Wisdom teeth are the third molars that erupt in the back of the mouth. They often erupt in a crowded or misaligned position, leading to pain, infection, or damage to other teeth. Insurance coverage for wisdom tooth removal is usually based on medical necessity.
- Simple Wisdom Tooth Removal: This involves removing a wisdom tooth that has erupted fully and is visible above the gum line. It is often covered when the tooth is causing pain, infection, or other complications.
- Surgical Wisdom Tooth Removal: This involves removing a wisdom tooth that is impacted (trapped below the gum line or bone), broken, or otherwise difficult to remove. It is often covered when the tooth is causing pain, infection, or other complications.
For example, if your wisdom teeth are causing pain, infection, or other problems, your insurance may cover the cost of removal.
Other Covered Procedures
In addition to the procedures listed above, other oral surgeries may be covered by health insurance, depending on your specific plan and the circumstances. These procedures may include:
- Cleft Palate Repair: This involves surgically correcting a cleft palate, a birth defect that affects the roof of the mouth.
- Temporomandibular Joint (TMJ) Surgery: This involves surgically treating problems with the jaw joint, such as pain, clicking, or locking.
- Orthognathic Surgery: This involves surgically correcting jaw deformities, such as an underbite or overbite.
Uncommon or Excluded Procedures
While most common oral surgeries are covered by health insurance, certain procedures are less likely to be included in standard plans. These exclusions often stem from factors like the procedure’s perceived cosmetic nature, lack of proven medical necessity, or high costs.
Reasons for Exclusion
- Cosmetic Procedures: Many dental procedures aimed solely at improving aesthetics, such as teeth whitening, veneers, and cosmetic gum contouring, are typically considered elective and not covered by insurance.
- Lack of Medical Necessity: Procedures deemed unnecessary for maintaining oral health or addressing a medical condition are often excluded. For instance, some insurance plans may not cover procedures like dental implants if a bridge or denture could effectively address the issue.
- High Costs: Complex or extensive procedures, such as full-mouth reconstruction or advanced bone grafting, can be costly. Insurance companies might limit coverage for such procedures or impose high deductibles and copayments.
Examples of Uncommon or Excluded Procedures
- Implants for purely cosmetic reasons: While dental implants are often covered for functional purposes, insurance may not cover them when the sole reason is to improve the appearance of teeth.
- Orthodontic treatment for adults: Many insurance plans cover braces for children but may not cover them for adults unless there’s a documented medical necessity, such as TMJ disorders or severe bite problems.
- Sleep apnea devices: Although some plans cover oral appliances for sleep apnea, others may exclude them or require pre-authorization.
- Laser dentistry: Some laser procedures, such as gum reshaping or tooth whitening, are not always covered due to their perceived cosmetic nature and high costs.
Exceptions and Special Circumstances
- Medical Necessity: If a procedure is deemed medically necessary to address a health condition, insurance coverage is more likely. For example, dental implants may be covered if they’re needed to replace missing teeth and prevent further complications.
- Pre-existing Conditions: Some insurance plans may have specific provisions for covering certain procedures related to pre-existing conditions. For instance, a plan might cover oral surgery for a patient with a history of oral cancer.
- State Regulations: Some states have regulations that require insurance plans to cover specific dental procedures, regardless of their cosmetic nature.
Alternative Financing Options
- Dental Savings Plans: These plans allow individuals to save pre-tax dollars for dental expenses, including uncovered procedures.
- Health Savings Accounts (HSAs): If you have a high-deductible health plan, you can use an HSA to pay for eligible medical expenses, including some dental procedures.
- Payment Plans: Many dental offices offer financing options, such as payment plans or low-interest loans, to help patients afford uncovered procedures.
Navigating the Insurance Process: Will Health Insurance Cover Oral Surgery
Getting your oral surgery covered by health insurance can feel like navigating a maze, but understanding the process can make it much smoother. Here’s a breakdown of the key steps, tips for effective communication, and guidance on documentation and claims.
Understanding the Process
The process of getting oral surgery covered by health insurance typically involves several steps:
- Contact your insurance provider: Before scheduling surgery, reach out to your insurance company to discuss coverage. This will help you understand what’s covered, what your out-of-pocket costs might be, and if pre-authorization is required.
- Obtain pre-authorization: In many cases, your insurance provider may require pre-authorization for certain procedures. This means you’ll need to submit a request to your insurance company for approval before the surgery.
- Schedule your surgery: Once you have pre-authorization (if required) and understand your coverage, you can schedule your surgery with your oral surgeon.
- Receive treatment: On the day of your surgery, be sure to bring your insurance card and any necessary documentation, such as your pre-authorization approval.
- File your claim: After your surgery, your oral surgeon will submit a claim to your insurance provider for reimbursement.
- Review your Explanation of Benefits (EOB): Once your claim is processed, you’ll receive an EOB detailing the amount your insurance paid and any remaining balance you owe.
Communicating Effectively with Your Insurance Provider
Clear communication is crucial for a smooth insurance experience. Here are some tips:
- Keep detailed records: Keep track of all your communications with your insurance provider, including dates, times, and the names of anyone you spoke with.
- Be clear and concise: When speaking to your insurance provider, be clear about your questions and concerns. Use simple language and avoid jargon.
- Request everything in writing: Whenever possible, request written confirmation of any agreements or decisions made with your insurance provider. This helps prevent misunderstandings and provides documentation for future reference.
- Be persistent: If you encounter any issues or delays, don’t be afraid to follow up with your insurance provider. Persistence can help ensure your claim is processed promptly.
Pre-Authorization Requirements
Pre-authorization is a process that involves getting approval from your insurance provider before undergoing certain procedures. This helps ensure that the procedure is medically necessary and covered by your insurance plan.
- Documentation: The specific documentation required for pre-authorization can vary depending on your insurance provider and the procedure. However, common documents include:
- A referral from your primary care physician
- A detailed medical history
- A description of the proposed procedure
- Supporting medical records
- Timeframe: It’s important to submit your pre-authorization request well in advance of your planned surgery date. Processing times can vary, so allow ample time for approval.
Filing Claims and Resolving Disputes
Once your surgery is complete, your oral surgeon will submit a claim to your insurance provider for reimbursement.
- Claim process: The claim process typically involves providing your insurance information and details about the procedure. Your insurance provider will then review the claim and determine the amount they will pay.
- Disputes: If your claim is denied or you disagree with the amount your insurance provider is paying, you have the right to appeal the decision.
- Gather evidence: To support your appeal, gather any relevant documentation, such as medical records, bills, and correspondence with your insurance provider.
- Follow the appeal process: Your insurance provider will have a specific process for appealing claims. Be sure to follow their instructions carefully.
- Consider seeking professional help: If you’re having difficulty navigating the appeal process, you may want to consider seeking help from a consumer advocate or a lawyer specializing in insurance law.
Ultimate Conclusion

Navigating the world of oral surgery and insurance can be a complex process. However, by understanding the key factors that influence coverage, the potential out-of-pocket costs, and the steps involved in getting pre-authorization, you can make informed decisions about your oral health care. Remember, proactive communication with your insurance provider and thorough research into different plans can help you secure the coverage you need and minimize unexpected financial burdens.
FAQ Summary
What are some examples of oral surgeries typically covered by health insurance?
Commonly covered oral surgeries include wisdom teeth removal, tooth extractions, bone grafts, and some types of dental implants. However, specific coverage varies by insurance plan.
Do I need pre-authorization for all oral surgeries?
Pre-authorization is often required for oral surgeries, especially more complex procedures. Contact your insurance provider to confirm whether pre-authorization is necessary for your specific surgery.
How can I minimize out-of-pocket costs for oral surgery?
Consider factors like deductibles and copayments when choosing an insurance plan. Additionally, explore options like dental savings accounts (DSAs) or health savings accounts (HSAs) to help cover out-of-pocket expenses.