- Understanding Breast Reduction Surgery
- Health Insurance Coverage for Breast Reduction
- Factors Influencing Coverage
- Navigating the Insurance Process
- Financial Considerations: Will Health Insurance Cover Breast Reduction
- Alternatives to Insurance Coverage
- Patient Rights and Advocacy
- Last Point
- Questions Often Asked
Will health insurance cover breast reduction? It’s a question many women considering this procedure ask. While breast reduction surgery can be life-changing, navigating the insurance process can feel overwhelming. This guide explores the factors that influence coverage decisions, offering insights into what you need to know before scheduling surgery.
Understanding the medical necessity for breast reduction is crucial. Insurance companies typically cover this procedure when it addresses health concerns like back pain, neck pain, or skin irritation caused by excessive breast size. They also consider factors like your overall health, pre-existing conditions, and the specific type of surgery required.
Understanding Breast Reduction Surgery

Breast reduction surgery, also known as reduction mammaplasty, is a procedure that removes excess breast tissue, fat, and skin to reduce the size and weight of the breasts. It is often performed for both medical and aesthetic reasons.
Medical Reasons for Breast Reduction Surgery
Breast reduction surgery can be medically necessary to alleviate a variety of physical problems associated with large breasts, such as:
- Back pain: Large breasts can put significant strain on the back muscles, leading to chronic pain and discomfort.
- Neck pain: The weight of large breasts can also cause neck pain and headaches.
- Shoulder pain: Large breasts can make it difficult to wear certain types of clothing and can also lead to shoulder pain.
- Skin irritation: Large breasts can cause skin irritation and rashes due to chafing and moisture.
- Limited physical activity: The weight and size of large breasts can make it difficult to participate in certain types of physical activities, such as running or swimming.
- Difficulty breathing: In some cases, large breasts can make it difficult to breathe, especially when lying down.
- Psychological distress: Large breasts can also cause psychological distress, leading to low self-esteem and social anxiety.
Types of Breast Reduction Procedures
There are several different types of breast reduction procedures, and the best option for you will depend on your individual needs and goals.
- Periareolar incision: This technique involves making an incision around the areola, which is the dark area around the nipple. This is the most common type of breast reduction surgery and is typically used for smaller reductions.
- Vertical incision: This technique involves making an incision from the areola down to the crease below the breast. This is used for larger reductions and can be combined with a periareolar incision.
- Inverted T incision: This technique involves making an incision that resembles an inverted T, with a vertical incision from the areola down to the crease below the breast and a horizontal incision across the crease. This is used for very large reductions.
Recovery Process and Potential Complications
After breast reduction surgery, you will need to wear a compression bra for several weeks to help reduce swelling and support the breasts. You will also need to avoid strenuous activity for several weeks.
- Potential complications: Like any surgery, breast reduction surgery carries some risks of complications. These can include infection, bleeding, bruising, scarring, and asymmetry.
- Numbness: Numbness in the breasts is a common side effect of breast reduction surgery, but it usually resolves over time.
- Swelling: Swelling is also common after breast reduction surgery and can last for several weeks. You can help reduce swelling by wearing a compression bra and elevating your breasts.
- Pain: You will likely experience some pain after surgery, which can be managed with pain medication. The pain should gradually decrease over time.
Health Insurance Coverage for Breast Reduction

While breast reduction surgery can significantly improve a person’s quality of life, it is often considered a cosmetic procedure by insurance companies. This means that coverage is not guaranteed and will depend on several factors, including medical necessity.
Determining Medical Necessity
Insurance companies evaluate the medical necessity of breast reduction surgery based on a comprehensive assessment of the patient’s physical and mental health. This evaluation typically involves a review of the patient’s medical history, physical examination, and diagnostic testing.
“Insurance companies typically require documentation of the patient’s symptoms and how those symptoms impact their daily life.”
Factors Influencing Coverage Decisions
Several factors can influence an insurance company’s decision regarding coverage for breast reduction surgery. These include:
- Severity of Symptoms: The presence of severe physical symptoms, such as back pain, neck pain, or skin irritation, is often a key factor in determining coverage. Documentation of these symptoms, including their impact on daily life, is crucial.
- Psychological Impact: The psychological impact of large breasts, such as depression, anxiety, or social isolation, is also considered. Mental health professionals may provide assessments and recommendations to support the claim.
- Pre-existing Conditions: Individuals with pre-existing conditions, such as obesity or certain musculoskeletal disorders, may face challenges in obtaining coverage. Insurance companies may require additional documentation to assess the role of these conditions in the decision-making process.
- Age: Some insurance policies may have age restrictions for coverage of breast reduction surgery. For example, policies may require the patient to be a certain age before approving the procedure.
Factors Influencing Coverage
While breast reduction surgery can provide significant physical and psychological benefits, insurance coverage is often a major concern. Insurance companies generally base their coverage decisions on a combination of factors, including medical necessity, policy terms, and state regulations.
Medical Necessity
The primary factor influencing insurance coverage for breast reduction surgery is medical necessity. Insurance companies typically cover procedures that are deemed medically necessary to treat a health condition or prevent future health problems.
For breast reduction, medical necessity is often established based on:
- Physical discomfort and pain: Large breasts can cause back pain, neck pain, shoulder pain, and difficulty breathing.
- Skin irritation and infections: The weight of large breasts can lead to skin irritation, rashes, and infections under the breasts.
- Limited mobility and physical activity: Large breasts can restrict movement and make it difficult to participate in physical activities.
- Psychological distress: Large breasts can cause body image issues, low self-esteem, and social anxiety.
To determine medical necessity, insurance companies may require documentation from a qualified medical professional, such as a surgeon, physician, or psychologist. This documentation typically includes a detailed medical history, physical examination findings, and a clear explanation of how the surgery will address the patient’s medical condition.
Coverage Policies of Different Insurance Providers
Insurance coverage policies vary significantly among different insurance providers. Some insurers may have more comprehensive coverage for breast reduction surgery, while others may have more limited coverage or may require specific criteria to be met. It is essential to review your insurance policy carefully to understand your coverage and any limitations.
Here are some key aspects of coverage policies that you should consider:
- Pre-authorization requirements: Some insurance providers require pre-authorization for breast reduction surgery. This means that you must obtain approval from your insurer before the surgery can be performed.
- Coverage for specific medical conditions: Some insurers may only cover breast reduction surgery for specific medical conditions, such as severe back pain or skin infections.
- Out-of-pocket costs: Even if your insurance covers breast reduction surgery, you may still be responsible for out-of-pocket costs, such as copayments, deductibles, and coinsurance.
- Network restrictions: Your insurance plan may have a network of providers, which means that you may only be covered for surgery performed by surgeons within that network.
Impact of State Regulations
State regulations can also play a role in insurance coverage for breast reduction surgery. Some states have laws that require insurance companies to cover breast reduction surgery when it is medically necessary, while others have no such laws. It is important to research the specific regulations in your state to understand your rights and options.
For example, some states have laws that require insurance companies to cover breast reduction surgery for women with severe back pain or other physical problems caused by large breasts. However, these laws may have specific requirements, such as the need for a specific diagnosis or a minimum breast size.
It is also important to note that state regulations can change over time. It is always best to consult with your insurance provider and a qualified medical professional to obtain the most up-to-date information on coverage and regulations.
Navigating the Insurance Process
Getting pre-authorization for breast reduction surgery is a crucial step in ensuring your insurance coverage. It involves a series of procedures and communication with your insurance provider. Understanding these steps and navigating the process effectively can help you maximize your chances of approval and avoid unexpected costs.
Pre-Authorization Process
Pre-authorization, also known as prior authorization, is a process where your insurance company reviews your medical necessity for the procedure before you undergo it. This ensures that the surgery is deemed medically necessary and falls within your insurance plan’s coverage guidelines. The process typically involves these steps:
- Your Doctor’s Referral: Your doctor will submit a pre-authorization request to your insurance company. This request includes your medical history, physical examination findings, and the rationale for recommending breast reduction surgery.
- Insurance Review: Your insurance company will review the request, considering your medical history, diagnosis, and the surgery’s necessity. They may also require additional information, such as medical records or supporting documentation.
- Decision: After the review, your insurance company will make a decision regarding pre-authorization. They may approve the surgery, approve it with certain conditions, or deny it altogether.
- Appeal: If your pre-authorization is denied, you have the right to appeal the decision. This involves submitting additional information or documentation to support your case.
Communicating with Your Insurance Provider
Clear and effective communication with your insurance provider is crucial throughout the pre-authorization process. Here are some key points to keep in mind:
- Be Proactive: Reach out to your insurance provider early in the process to inquire about pre-authorization requirements and deadlines. This allows you to gather the necessary documentation and avoid delays.
- Be Clear and Concise: When communicating with your insurance provider, use clear and concise language. Provide all the necessary information and address any questions they may have promptly.
- Keep Records: Document all communication with your insurance provider, including dates, times, and the content of conversations. This helps you track the process and avoid misunderstandings.
- Understand Your Policy: Carefully review your insurance policy to understand your coverage limits, pre-authorization procedures, and any exclusions that might apply to breast reduction surgery.
Gathering Key Documents
Having the necessary documents readily available can streamline the pre-authorization process and minimize delays. These documents are essential:
- Doctor’s Referral: This is the initial request from your doctor outlining the medical necessity for breast reduction surgery.
- Medical Records: These include your medical history, past surgeries, and any relevant diagnostic tests.
- Supporting Documentation: This may include photographs, medical reports, or other documentation that supports the need for breast reduction surgery.
- Insurance Policy: Keep your insurance policy handy to refer to coverage details, pre-authorization procedures, and any exclusions that may apply.
- Pre-Authorization Form: This form is typically provided by your insurance company and needs to be completed by your doctor and submitted with other supporting documentation.
Financial Considerations: Will Health Insurance Cover Breast Reduction
Breast reduction surgery, while potentially life-changing, comes with significant financial implications. Understanding these costs and exploring available financing options can help you make informed decisions about your procedure.
Out-of-Pocket Costs, Will health insurance cover breast reduction
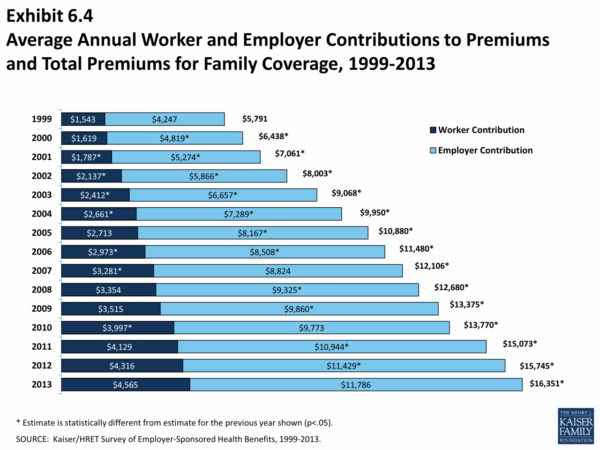
Out-of-pocket costs for breast reduction can vary widely based on factors such as your location, surgeon’s fees, anesthesia costs, facility fees, and post-operative care. Here’s a breakdown of potential expenses:
- Surgeon’s Fees: This is typically the largest expense, ranging from a few thousand dollars to over $10,000 depending on the surgeon’s experience and the complexity of the procedure.
- Anesthesia Fees: These costs vary depending on the type of anesthesia used and the duration of the procedure.
- Facility Fees: This covers the use of the operating room and other medical equipment.
- Post-Operative Care: This includes follow-up appointments, medications, and any necessary supplies.
Financing Options
Several options can help you finance your breast reduction surgery:
- Health Savings Accounts (HSAs): These tax-advantaged accounts can be used for medical expenses, including breast reduction surgery, if it’s deemed medically necessary.
- Flexible Spending Accounts (FSAs): Similar to HSAs, these accounts allow you to set aside pre-tax dollars for medical expenses, including breast reduction surgery, if it’s medically necessary.
- Medical Loans: These loans offer financing options specifically for medical procedures, often with lower interest rates than personal loans.
- Payment Plans: Some surgeons and facilities offer payment plans to help patients manage the costs of surgery.
Tax Benefits
Medical expenses exceeding a certain percentage of your Adjusted Gross Income (AGI) can be deducted on your federal income taxes. For example, if your AGI is $50,000 and your medical expenses exceed $5,000, you can deduct the amount exceeding $5,000. This deduction can help offset some of the financial burden associated with breast reduction surgery.
Alternatives to Insurance Coverage

If your health insurance doesn’t cover breast reduction surgery, or if you have a high deductible or co-pay, you might need to explore alternative funding sources. Here are some options to consider.
Crowdfunding
Crowdfunding platforms allow individuals to raise money from a large number of people, often through online platforms.
- Websites like GoFundMe, Kickstarter, and Indiegogo allow you to create a campaign and share your story with potential donors.
- These platforms often allow you to set a fundraising goal and track your progress.
- You can share your campaign on social media and with your network to increase visibility.
However, it’s important to note that crowdfunding can be unpredictable, and there’s no guarantee that you’ll reach your fundraising goal.
Medical Loans and Payment Plans
Medical loans are designed to help people pay for medical expenses that are not covered by insurance.
- Banks, credit unions, and online lenders offer medical loans with varying interest rates and repayment terms.
- Some medical providers offer payment plans, which allow you to pay for the surgery in installments.
- Before taking out a loan, compare interest rates and terms from different lenders to find the best option for you.
Financial Assistance Programs
Several organizations offer financial assistance for medical procedures, including breast reduction surgery.
- The Patient Advocate Foundation (PAF) provides free case management and financial assistance to patients facing medical hardship.
- The National Breast Cancer Foundation (NBCF) offers financial assistance to women diagnosed with breast cancer, which may cover the cost of breast reduction surgery in some cases.
- Some hospitals and clinics have their own financial assistance programs for patients who meet certain criteria.
It’s important to research available programs and contact organizations directly to inquire about eligibility requirements and application procedures.
Patient Rights and Advocacy
You have the right to understand your insurance coverage and to advocate for yourself when it comes to accessing necessary healthcare. This includes breast reduction surgery if it’s medically necessary. Patient advocacy groups play a crucial role in supporting individuals navigating the complexities of healthcare systems.
Patient Rights Related to Insurance Coverage
Understanding your rights is essential when dealing with insurance companies. Here’s a breakdown of key patient rights:
- Right to Access Medical Records: You have the right to review and obtain copies of your medical records. This information can be vital in supporting your case for coverage.
- Right to Appeal Denials: If your insurance company denies coverage for breast reduction surgery, you have the right to appeal the decision. The appeals process can be complex, but patient advocacy groups can provide guidance.
- Right to Confidentiality: Your medical information is confidential and protected under HIPAA (Health Insurance Portability and Accountability Act). Insurance companies are obligated to maintain the privacy of your medical records.
- Right to Choose Providers: You have the right to choose your healthcare providers, including surgeons, within your insurance network. This ensures you receive care from someone you trust.
Role of Patient Advocacy Groups
Patient advocacy groups play a crucial role in supporting individuals seeking healthcare, including breast reduction surgery. They offer a variety of resources and support, including:
- Information and Education: Advocacy groups provide valuable information about insurance coverage, patient rights, and the surgical process.
- Support and Guidance: They offer emotional support and guidance throughout the process, helping individuals navigate complex insurance procedures and appeals.
- Advocacy and Lobbying: Advocacy groups advocate for policies that improve access to healthcare, including breast reduction surgery, and lobby for changes to insurance regulations.
Appealing an Insurance Denial
If your insurance company denies coverage for breast reduction surgery, you have the right to appeal the decision. The appeals process typically involves the following steps:
- Review the Denial Letter: Carefully review the denial letter to understand the reason for the denial. This will help you prepare your appeal.
- Gather Supporting Documentation: Collect all relevant medical records, including your doctor’s recommendations, medical evaluations, and any other supporting documentation.
- File an Appeal: Submit a formal appeal to your insurance company, clearly outlining the reasons why you believe the denial should be overturned. Be sure to include all supporting documentation.
- Consider an Independent Medical Review: If your initial appeal is denied, you may be able to request an independent medical review by a qualified physician. This can provide an unbiased opinion on the medical necessity of the surgery.
Last Point
While navigating the insurance process for breast reduction can be complex, understanding your options and advocating for yourself can make a difference. By familiarizing yourself with the criteria for coverage, communicating effectively with your insurance provider, and exploring alternative funding sources, you can take control of your healthcare journey and achieve your desired outcome.
Questions Often Asked
What are the most common reasons for breast reduction?
Common reasons include back pain, neck pain, skin irritation, difficulty with physical activity, and psychological distress.
How can I increase my chances of insurance coverage?
Gather detailed medical documentation from your doctor, including a clear explanation of your medical necessity for the procedure. Also, consider seeking a second opinion from a specialist to strengthen your case.
What if my insurance denies coverage for breast reduction?
You have the right to appeal the denial. Carefully review the reasons for denial and gather additional medical evidence to support your appeal. Consider contacting a patient advocacy group for assistance.