Does my health insurance cover mental health? This is a question that many people ask, and the answer can vary depending on your specific plan. Understanding the nuances of mental health coverage is crucial, as it can significantly impact your access to essential services.
Mental health coverage can be complex, with various types of plans offering different levels of benefits. From basic coverage that may only include a limited number of therapy sessions to comprehensive plans that provide extensive services, it’s important to know what your plan offers.
Understanding Health Insurance Coverage: Does My Health Insurance Cover Mental Health

Navigating the world of health insurance can be overwhelming, especially when it comes to mental health coverage. Understanding the different types of plans and their benefits is crucial to ensuring you have adequate support when you need it.
Types of Health Insurance Plans
The United States offers a variety of health insurance plans, each with its own structure and coverage. Here are some common types of plans and their typical mental health benefits:
- Individual Health Insurance Plans: These plans are purchased directly by individuals, often through the Health Insurance Marketplace. Coverage varies depending on the plan, but generally includes some mental health benefits.
- Employer-Sponsored Health Insurance Plans: Many employers offer health insurance plans to their employees. These plans often have more robust mental health benefits than individual plans.
- Medicaid: This government-funded program provides health insurance to low-income individuals and families. Medicaid covers mental health services, including therapy and medication.
- Medicare: This government-funded program provides health insurance to individuals aged 65 and older, as well as people with certain disabilities. Medicare Part B covers some mental health services, while Medicare Advantage plans may offer more comprehensive coverage.
Mental Health Coverage Tiers
Mental health coverage can be divided into different tiers, each offering varying levels of benefits:
- Basic Coverage: This tier typically includes a limited number of mental health visits per year, with copayments or coinsurance. It may have a lower maximum out-of-pocket cost for mental health services.
- Enhanced Coverage: This tier offers more comprehensive mental health benefits, including a higher number of visits, lower copayments, and a broader range of services. It may also have a higher maximum out-of-pocket cost.
- Comprehensive Coverage: This tier provides the most extensive mental health benefits, with unlimited visits, low copayments, and a wide range of services. It may have a higher monthly premium but offers the greatest peace of mind.
Common Health Insurance Plans and Mental Health Benefits
Here are some examples of common health insurance plans and their typical mental health benefits:
| Plan Type | Typical Mental Health Benefits |
|---|---|
| HMO (Health Maintenance Organization) | Often require you to choose a primary care physician (PCP) who will refer you to mental health providers within the network. May have lower premiums but limited out-of-network coverage. |
| PPO (Preferred Provider Organization) | Offer more flexibility to see providers outside of the network, but typically have higher premiums and copayments. |
| POS (Point-of-Service) | Combine elements of HMO and PPO plans. May require you to choose a PCP for referrals, but offer some out-of-network coverage. |
It’s important to note that specific coverage details, including the number of visits, copayments, and out-of-pocket costs, can vary significantly between plans. It’s crucial to carefully review your plan’s benefits and limitations before making a decision.
Key Mental Health Benefits
Most health insurance plans include coverage for mental health services, but the specific benefits and limitations can vary greatly. It’s crucial to understand what your plan covers and how to access these services.
Mental health benefits are designed to help individuals manage and treat a wide range of mental health conditions. These benefits typically include:
Therapy Sessions
Therapy sessions are a fundamental component of mental health care. They provide a safe and confidential space for individuals to discuss their concerns, develop coping mechanisms, and work towards their mental well-being. Health insurance plans typically cover therapy sessions with licensed mental health professionals, such as psychologists, psychiatrists, and social workers.
However, there are often limitations on the number of sessions covered. For instance, some plans may have a pre-determined limit on the number of sessions per year, while others may require pre-authorization for each session. Additionally, network restrictions may limit access to specific therapists or require individuals to seek treatment within a designated network of providers.
Medication
Medication can be an essential part of managing certain mental health conditions. Health insurance plans generally cover prescription medications for mental health conditions, but there are often limitations on the types of medications covered and the quantity dispensed.
Some plans may require pre-authorization for certain medications or may have a formulary, which lists the specific medications covered. Additionally, copayments or coinsurance may apply to prescription medications.
Inpatient Care
Inpatient care is necessary for individuals experiencing severe mental health crises or requiring intensive treatment. Health insurance plans typically cover inpatient care at psychiatric hospitals or specialized mental health facilities.
However, there may be limits on the length of stay or specific criteria that must be met for coverage. For example, some plans may require a specific diagnosis or a certain level of severity before approving inpatient care. Additionally, network restrictions may apply to inpatient facilities.
Coverage Differences for Mental Health Conditions
The coverage for different mental health conditions can vary. For example, some plans may provide more extensive coverage for anxiety and depression than for substance abuse or eating disorders.
It’s important to review your health insurance plan’s specific coverage details to understand the benefits and limitations for each mental health condition.
Factors Influencing Coverage

The extent of mental health coverage you receive can vary significantly depending on a range of factors, including state laws, insurance provider, and your employer’s plan. Understanding these factors can help you make informed decisions about your health insurance choices.
State Laws and Regulations
State laws play a crucial role in shaping mental health coverage. Many states have enacted parity laws, which require insurance plans to cover mental health services at the same level as medical and surgical benefits. These laws help ensure that individuals with mental health conditions receive equitable access to care. However, the specific requirements and scope of parity laws can vary from state to state. For instance, some states may have stronger parity laws that include coverage for specific types of mental health services, such as addiction treatment or eating disorder care.
Insurance Provider Differences
Mental health coverage can differ significantly between insurance providers. Even within the same state, different insurance companies may offer varying levels of benefits, deductibles, and copayments for mental health services. Some insurance providers may have more extensive networks of mental health professionals, while others may have limited options in certain geographic areas.
It’s essential to compare the mental health benefits offered by different insurance providers before making a decision.
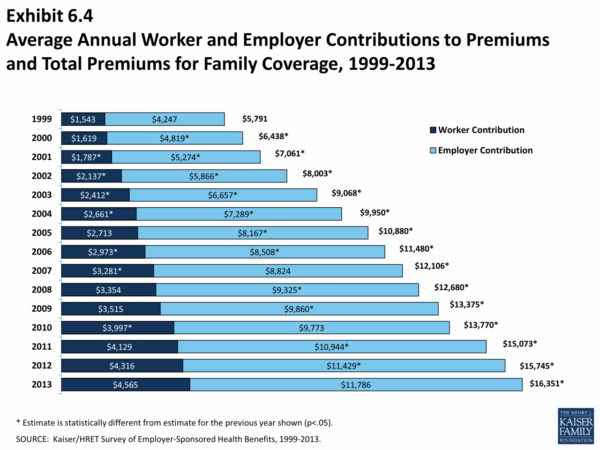
Employer-Sponsored Health Insurance Plans
Employer-sponsored health insurance plans are a common source of mental health coverage. These plans can offer unique features and limitations, depending on the employer’s specific policies and the chosen insurance provider. Some employers may provide additional mental health benefits, such as employee assistance programs (EAPs) or mental health wellness programs. However, it’s important to note that employer-sponsored plans may have specific limitations on the types of mental health services covered, such as the number of therapy sessions or the types of mental health professionals included in the network.
Accessing Mental Health Services
Once you understand your mental health coverage, you can start accessing services. This involves verifying your coverage, finding providers within your network, and navigating the pre-authorization process.
Verifying Mental Health Coverage
Before seeking mental health services, it’s crucial to confirm your coverage details. This ensures you understand what services are covered, the limitations, and any associated costs.
- Review your insurance plan documents: Carefully read your policy documents, including the summary of benefits, to understand your mental health coverage. Pay attention to the specific services covered, the annual or lifetime limits, and any deductibles or copayments.
- Contact your insurance provider: If you have any questions or need clarification about your coverage, reach out to your insurance provider’s customer service department. They can provide detailed information about your specific plan and answer any queries you may have.
- Use online tools: Many insurance companies offer online portals or mobile apps where you can access your policy documents, check coverage details, and find in-network providers.
Finding Mental Health Providers
Finding a qualified mental health professional within your network is essential for accessing services efficiently.
- Use your insurance provider’s directory: Most insurance companies have online directories or provider search tools that allow you to find mental health professionals within your network. These directories often provide information about the provider’s specialties, location, and contact details.
- Ask for recommendations: Reach out to your primary care physician, friends, family, or support groups for recommendations for mental health professionals in your area.
- Search online directories: Websites like Psychology Today and the American Psychological Association (APA) offer comprehensive directories of mental health professionals, including those who accept specific insurance plans.
Navigating the Pre-Authorization Process
Many insurance plans require pre-authorization for mental health services, meaning you need to obtain approval from your insurance company before receiving treatment.
- Understand the process: Contact your insurance provider to inquire about their pre-authorization process. Ask about the required documentation, deadlines, and any specific forms that need to be completed.
- Obtain the necessary information: Gather all the required information, including your insurance details, the provider’s information, and a detailed description of the requested services.
- Submit the pre-authorization request: Complete and submit the pre-authorization request form to your insurance provider through their designated channels, such as mail, fax, or online portal.
- Follow up: After submitting the request, follow up with your insurance provider to track its status and ensure timely approval.
Resources and Tools for Accessing Mental Health Care
Several resources and tools can assist you in understanding your coverage and accessing mental health care:
- Mental Health America (MHA): MHA offers a wealth of information on mental health, including resources on insurance coverage, finding providers, and navigating the healthcare system.
- National Alliance on Mental Illness (NAMI): NAMI provides support and advocacy for individuals with mental illness and their families. They offer resources on insurance coverage, finding treatment, and navigating the healthcare system.
- The Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA offers a directory of mental health and substance abuse treatment facilities and resources, including information on insurance coverage.
Financial Considerations

While mental health coverage is crucial, it’s essential to understand the potential financial implications. Understanding out-of-pocket costs and available resources can help you make informed decisions about your mental health care.
Out-of-Pocket Costs
Out-of-pocket costs are expenses you pay directly for mental health services. These costs can vary depending on your insurance plan and the specific services you receive.
- Copayments: A fixed amount you pay each time you receive a service, such as a therapy session.
- Deductibles: The amount you pay before your insurance starts covering costs.
- Coinsurance: A percentage of the cost you pay after your deductible is met.
Financial Implications of Different Treatment Options
The financial implications of mental health treatment vary depending on the type of service you need.
- Therapy: Therapy sessions typically involve copayments or coinsurance. The cost can vary depending on the therapist’s fees and your insurance plan.
- Medication: Prescription medications for mental health conditions can be expensive, but your insurance plan may cover a portion of the cost. You may also have to pay a copayment or coinsurance for each prescription.
- Inpatient Care: Inpatient treatment at a mental health facility can be very costly, but your insurance plan may cover a significant portion of the expenses. However, you may still have to pay a deductible or coinsurance.
Managing Mental Health Care Costs, Does my health insurance cover mental health
Several resources can help you manage the cost of mental health care.
- Financial Assistance Programs: Some organizations offer financial assistance to help people afford mental health care. For example, the National Alliance on Mental Illness (NAMI) offers a variety of resources, including financial assistance programs.
- Sliding-Scale Fees: Some mental health providers offer sliding-scale fees, which means they charge based on your ability to pay.
- Negotiating with Providers: You can sometimes negotiate with mental health providers to reduce their fees. This may be possible if you have a limited income or are facing financial hardship.
Conclusive Thoughts
Navigating the world of mental health insurance can feel daunting, but it’s essential to be informed. By understanding your coverage, you can make informed decisions about your care and advocate for the services you need. Remember, seeking mental health support is a sign of strength, and access to affordable care is a fundamental right.
General Inquiries
How do I know if my health insurance covers mental health?
The best way to determine your mental health coverage is to contact your insurance provider directly. They can provide you with a detailed explanation of your plan’s benefits and any limitations.
What if my insurance plan doesn’t cover mental health?
If your plan doesn’t cover mental health services, there are still options available. You can explore other insurance plans that offer mental health coverage, or you can seek out affordable mental health clinics and organizations that provide services on a sliding-scale fee basis.
What are some common mental health conditions covered by insurance?
Common mental health conditions covered by insurance plans include anxiety, depression, bipolar disorder, PTSD, and substance abuse. However, coverage may vary depending on your specific plan.