Can an employer pay 100 of health insurance – Can an employer pay 100% of health insurance? This question sparks curiosity about the intricate relationship between employers and employees in the realm of healthcare. Navigating the complexities of employer-sponsored health insurance plans, particularly the financial aspects, reveals a dynamic landscape shaped by legal frameworks, cost-sharing arrangements, and evolving market trends. This exploration delves into the factors influencing an employer’s decision to offer coverage, the legal considerations surrounding such plans, and the strategies employed by employers to manage costs.
Understanding the dynamics of employer-sponsored health insurance is crucial for both employers and employees. For employers, it involves navigating the legal requirements, balancing costs, and attracting and retaining talent. For employees, it means making informed decisions about their health insurance options and understanding their financial responsibilities. This journey through the world of employer-sponsored health insurance provides valuable insights into the factors shaping this critical aspect of the employment landscape.
Employer-Sponsored Health Insurance Basics
Employer-sponsored health insurance is a common benefit offered by many companies to their employees. It allows employees to access health insurance coverage at a lower cost than they would typically pay on their own. This type of insurance is often provided through group plans, where the employer negotiates with an insurance company to provide coverage for its employees.
Types of Employer-Sponsored Health Insurance Plans
There are several different types of employer-sponsored health insurance plans available, each with its own set of benefits and drawbacks. Here are some common examples:
- Health Maintenance Organization (HMO): HMOs typically offer lower premiums but restrict you to seeing doctors and specialists within their network. They usually require a referral from your primary care physician to see a specialist.
- Preferred Provider Organization (PPO): PPOs offer more flexibility than HMOs, allowing you to see doctors and specialists both in and out of their network. However, you’ll pay higher premiums and out-of-pocket costs for services received outside the network.
- Point of Service (POS): POS plans combine elements of HMOs and PPOs. They offer a network of providers, but you can also see out-of-network doctors for a higher cost.
- Exclusive Provider Organization (EPO): EPOs are similar to HMOs, but they allow you to see out-of-network providers for emergency care or when your primary care physician can’t provide the necessary treatment. However, you’ll pay higher out-of-pocket costs for out-of-network services.
- High Deductible Health Plan (HDHP): HDHPs have high deductibles, meaning you’ll pay a significant amount out-of-pocket before your insurance kicks in. However, they often come with lower premiums and may be combined with a Health Savings Account (HSA) to help you save money on healthcare costs.
Benefits and Drawbacks of Employer-Sponsored Health Insurance
Benefits for Employers
- Attracting and Retaining Employees: Offering health insurance can be a major draw for potential employees and help retain existing ones. This can improve employee morale and productivity.
- Tax Advantages: Employers can deduct the cost of providing health insurance as a business expense, which can save them money on taxes.
- Negotiated Rates: Group plans often provide lower premiums than individual plans, allowing employers to save money on healthcare costs.
Benefits for Employees
- Lower Premiums: Group plans typically offer lower premiums than individual plans, making health insurance more affordable for employees.
- Access to Comprehensive Coverage: Employer-sponsored plans often provide comprehensive coverage for a wide range of medical services, including preventive care, hospital stays, and prescription drugs.
- Tax Advantages: Premiums paid by employees are often tax-deductible, further reducing their healthcare costs.
Drawbacks for Employers
- Rising Healthcare Costs: Employers are often responsible for a significant portion of healthcare costs, which can increase over time.
- Administrative Burden: Managing a health insurance plan can be time-consuming and complex, requiring employers to handle paperwork, enrollment, and claims processing.
- Employee Health Concerns: Employers may face increased costs if their employees have significant health issues. This can lead to unpredictable expenses and potential budget constraints.
Drawbacks for Employees
- Limited Choice: Employees may have limited choices in terms of health insurance plans offered by their employer.
- Potential for Higher Out-of-Pocket Costs: Depending on the plan, employees may still face significant out-of-pocket costs for medical services.
- Loss of Coverage: If an employee loses their job, they may lose their health insurance coverage, potentially leading to a gap in coverage and increased costs.
Legal Considerations
Offering health insurance to employees comes with a set of legal requirements and regulations. Understanding these legal considerations is crucial for employers to avoid potential legal issues and ensure compliance.
The Affordable Care Act (ACA)
The ACA has significantly impacted employer-sponsored health insurance. It introduced various provisions, including:
- The Employer Shared Responsibility Provision: Employers with 50 or more full-time equivalent employees are required to offer affordable health insurance to their employees. Failure to do so can result in financial penalties.
- Minimum Value Requirements: The ACA mandates that employer-sponsored health insurance plans must meet minimum value standards, meaning they must cover a certain percentage of healthcare costs.
- Essential Health Benefits: The ACA requires that employer-sponsored health insurance plans cover a set of essential health benefits, including preventive care, maternity care, and prescription drugs.
- Premium Tax Credits: The ACA provides tax credits to individuals who purchase health insurance through the marketplace. These credits can reduce the cost of health insurance for employees who choose to purchase insurance outside of their employer’s plan.
Cost Sharing and Contribution
Employer-sponsored health insurance typically involves cost sharing between the employer and the employee. This means that both parties contribute to the overall cost of the insurance plan. Cost sharing helps to make health insurance more affordable for both employers and employees, while also encouraging individuals to be more mindful of their healthcare spending.
Cost Sharing Arrangements
Cost sharing arrangements are common in employer-sponsored health insurance plans and are designed to share the cost of healthcare services between the insurance company, the employer, and the employee. These arrangements help to keep premiums lower and encourage employees to be more conscious of their healthcare spending. Here are some common examples of cost-sharing arrangements:
- Deductible: The amount of money an individual must pay out-of-pocket before their health insurance coverage kicks in. For example, if your deductible is $1,000, you would need to pay the first $1,000 of your healthcare costs before your insurance starts covering the rest.
- Copayment: A fixed amount of money an individual pays for a specific healthcare service, such as a doctor’s visit or prescription drug. For example, you might have a $20 copayment for a doctor’s visit and a $10 copayment for a generic prescription drug.
- Coinsurance: A percentage of the cost of a healthcare service that an individual pays after meeting their deductible. For example, if your coinsurance is 20%, you would pay 20% of the cost of a healthcare service after you have met your deductible.
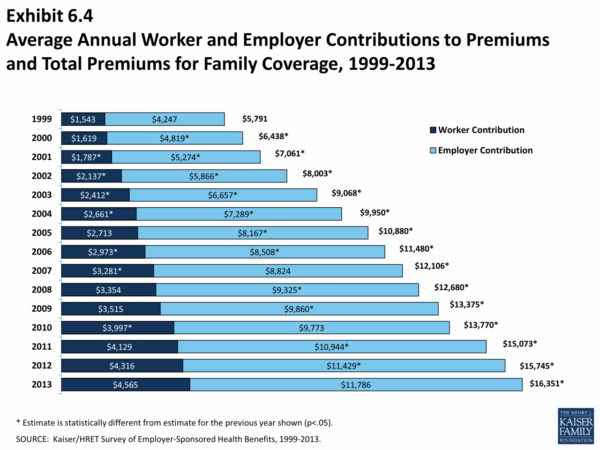
Employer and Employee Contributions
Employers and employees typically contribute to the cost of health insurance in different ways.
- Employer Contributions: Employers often contribute a significant portion of the cost of health insurance premiums. This contribution can take the form of a flat dollar amount or a percentage of the premium. The employer’s contribution helps to make health insurance more affordable for employees.
- Employee Contributions: Employees typically contribute a portion of the health insurance premium through payroll deductions. The employee’s contribution can vary depending on the type of plan chosen, the employee’s salary, and other factors. The employee’s contribution helps to share the cost of health insurance and encourages employees to be more engaged in choosing the right plan for their needs.
Factors Influencing Coverage
The decision of an employer to offer health insurance is influenced by a variety of factors, including company size, industry, and employee demographics. These factors play a crucial role in shaping the employer’s approach to providing health benefits, including the type of coverage offered, the level of benefits, and the cost-sharing arrangements.
Company Size and Industry
Company size and industry are significant factors in determining an employer’s ability and willingness to offer health insurance. Larger companies, with a larger pool of employees, are more likely to offer health insurance as it becomes more cost-effective to negotiate group rates with insurance providers. Smaller companies, on the other hand, may face higher costs per employee and may struggle to offer competitive benefits packages.
- Industry: Certain industries, such as healthcare, finance, and technology, typically offer more comprehensive health insurance benefits due to the competitive nature of the labor market and the need to attract and retain highly skilled employees. Industries with lower profit margins or those facing economic challenges may offer less generous benefits packages.
- Company Size: Large companies, with a significant workforce, can leverage their size to negotiate lower premiums and secure more favorable coverage options from insurance providers. Smaller companies may face higher premiums due to their smaller risk pool and limited bargaining power.
Employee Demographics
Employee demographics, including age, health status, and family size, also play a role in shaping an employer’s health insurance offering. Companies with a workforce that is predominantly older or has a higher prevalence of chronic conditions may face higher healthcare costs, leading to higher premiums. Conversely, companies with a younger workforce may face lower premiums due to lower healthcare utilization rates.
- Age: Older employees generally have higher healthcare costs due to an increased likelihood of chronic conditions. Companies with a predominantly older workforce may face higher premiums and may need to consider offering more comprehensive coverage to meet the needs of their employees.
- Health Status: Employees with pre-existing conditions or chronic illnesses may have higher healthcare utilization rates, leading to higher premiums. Companies may need to offer more comprehensive coverage to meet the needs of employees with pre-existing conditions.
- Family Size: Employees with dependents, such as spouses and children, will have higher healthcare costs. Companies may need to consider offering family coverage options to meet the needs of their employees and their families.
Premium Determination
Employee health insurance premiums are determined based on a variety of factors, including:
- Age and Gender: Insurance companies use actuarial data to assess the average healthcare costs associated with different age groups and genders.
- Location: Healthcare costs vary significantly across different geographic regions. Insurance companies adjust premiums to reflect the cost of living and healthcare utilization rates in specific areas.
- Coverage Options: The type and level of coverage offered by an employer’s health insurance plan will influence the premium. More comprehensive plans with higher benefit levels will typically have higher premiums.
- Risk Pool: The health status and demographics of the employee population within a company’s risk pool will also influence the premium. A risk pool with a higher prevalence of chronic conditions or older employees will generally have higher premiums.
- Claims History: Insurance companies consider the claims history of the employee population to assess the risk associated with a particular group. Companies with a history of high claims may face higher premiums.
Impact of Inflation and Economic Conditions
Inflation and economic conditions can have a significant impact on employer-sponsored health insurance. Rising healthcare costs due to inflation can lead to higher premiums, making it more expensive for employers to offer health insurance. Economic downturns can also impact employer-sponsored health insurance, as companies may reduce benefits or shift more costs to employees to control expenses.
- Inflation: Rising healthcare costs due to inflation can lead to higher premiums for employers. This can make it more challenging for employers to offer comprehensive health insurance benefits and may lead to increased cost-sharing for employees.
- Economic Downturn: During economic downturns, companies may reduce or eliminate health insurance benefits to control costs. Employers may also increase employee contributions to premiums or reduce the level of coverage offered.
Employer Strategies and Trends
Employers are constantly seeking ways to manage the rising costs of health insurance while providing competitive benefits to their employees. This has led to a shift in employer strategies, with a focus on cost-sharing, wellness programs, and innovative approaches like telehealth.
High-Deductible Health Plans (HDHPs) and Health Savings Accounts (HSAs)
HDHPs have become increasingly popular as employers seek to control costs. These plans have higher deductibles than traditional plans, but they offer lower monthly premiums. Employees with HDHPs can often open a Health Savings Account (HSA), which allows them to save pre-tax dollars to pay for healthcare expenses.
- Cost Savings for Employers: HDHPs typically have lower premiums for employers, helping them control costs.
- Employee Choice and Control: HSAs give employees more control over their healthcare spending, allowing them to save for future healthcare needs.
- Tax Advantages: Contributions to HSAs are tax-deductible, and withdrawals for qualified medical expenses are tax-free.
Wellness Programs and Disease Management Initiatives
Employers are increasingly investing in wellness programs and disease management initiatives to improve employee health and reduce healthcare costs. These programs can include:
- Health Education: Providing employees with information on healthy living, nutrition, and disease prevention.
- Fitness Programs: Offering gym memberships, fitness classes, or on-site fitness centers.
- Disease Management: Providing support and resources for employees with chronic conditions, such as diabetes or heart disease.
Telehealth and Virtual Care
Telehealth and virtual care are transforming healthcare delivery, and employers are embracing these technologies to offer more convenient and affordable healthcare options.
- Increased Access: Telehealth allows employees to consult with doctors remotely, reducing the need for in-person visits and making healthcare more accessible.
- Cost Reduction: Virtual care can reduce the cost of healthcare services, especially for routine appointments and follow-ups.
- Improved Convenience: Telehealth allows employees to access healthcare services at their convenience, without having to take time off work or travel.
Employee Considerations

Choosing the right health insurance plan is a crucial decision for employees, as it directly impacts their financial well-being and access to healthcare. Understanding the nuances of employer-sponsored health insurance is essential for making informed choices that align with individual needs and preferences.
Coverage Details, Can an employer pay 100 of health insurance
Employees should meticulously review the coverage details of each plan offered by their employer. This includes understanding key aspects such as deductibles, copayments, and out-of-pocket maximums. These components directly influence the financial responsibility employees bear for their healthcare expenses.
- Deductible: The amount an employee must pay out-of-pocket before insurance coverage kicks in for covered services. Higher deductibles often correspond to lower monthly premiums.
- Copayments: Fixed amounts employees pay for specific services, such as doctor visits or prescriptions, after meeting the deductible.
- Out-of-Pocket Maximum: The maximum amount an employee is required to pay for covered healthcare expenses in a given year. Once this limit is reached, insurance covers 100% of eligible costs.
Factors to Consider
Beyond coverage details, employees should consider several factors when evaluating health insurance options. These factors help them determine which plan best suits their individual circumstances and healthcare needs.
- Healthcare Needs: Evaluate individual and family healthcare needs, such as the frequency of doctor visits, prescription medication requirements, and potential need for specialized care. Choose a plan that provides adequate coverage for anticipated healthcare expenses.
- Network: Consider the network of healthcare providers included in each plan. Ensure that preferred doctors, hospitals, and specialists are within the network to avoid higher out-of-pocket costs for out-of-network services.
- Premiums: Compare the monthly premiums for each plan and consider the affordability in relation to individual income and budget. Higher premiums often translate to lower deductibles and copayments, while lower premiums may come with higher out-of-pocket costs.
- Benefits: Review the benefits offered by each plan, such as preventive care coverage, mental health services, and prescription drug coverage. Prioritize plans that provide comprehensive coverage for essential healthcare services.
- Flexibility: Consider the flexibility of each plan, such as options for choosing a primary care physician or the availability of telehealth services. Opt for plans that offer flexibility and convenience to meet individual needs.
Making Informed Decisions
Employees can make informed decisions about their health insurance choices by following these steps:
- Attend Employer Meetings: Participate in employer-sponsored meetings or presentations on health insurance options to gain a comprehensive understanding of the plans available.
- Review Plan Documents: Carefully read through the summary plan descriptions (SPDs) and evidence of coverage (EOC) documents provided by the employer. These documents contain detailed information about each plan’s coverage, costs, and benefits.
- Seek Expert Advice: Consult with a health insurance broker or financial advisor to gain personalized guidance and recommendations based on individual needs and financial circumstances.
- Compare Plans: Use online tools or resources to compare different health insurance plans side-by-side. This allows for a comprehensive analysis of coverage, costs, and benefits to make an informed decision.
- Ask Questions: Don’t hesitate to ask questions to the employer’s benefits department, insurance provider, or healthcare professionals to clarify any uncertainties or concerns about the plans.
Ultimate Conclusion: Can An Employer Pay 100 Of Health Insurance

The landscape of employer-sponsored health insurance is constantly evolving, driven by legal mandates, market forces, and technological advancements. Employers face the challenge of balancing cost management with employee satisfaction, while employees navigate a complex array of options and financial responsibilities. Understanding the interplay of these factors empowers both employers and employees to make informed decisions, ensuring access to quality healthcare while navigating the financial complexities of this critical benefit.
Popular Questions
What are the legal requirements for employers regarding health insurance?
The Affordable Care Act (ACA) mandates that employers with 50 or more full-time equivalent employees offer affordable health insurance to their employees or face penalties. There are exemptions for certain small businesses and religious employers.
Can employers deduct the cost of health insurance premiums from their taxes?
Yes, employers can deduct the cost of health insurance premiums as a business expense.
What are some common cost-sharing arrangements in employer-sponsored health insurance plans?
Common cost-sharing arrangements include deductibles, copayments, coinsurance, and out-of-pocket maximums. These arrangements require employees to share a portion of the healthcare costs.
What are some factors that influence an employer’s decision to offer health insurance?
Factors influencing an employer’s decision include company size, industry, employee demographics, and the competitive landscape.