- Understanding Open Enrollment Periods
- Special Enrollment Periods
- Enrollment Outside of Open Enrollment
- Consequences of Enrollment Outside Open Enrollment
- Navigating the Enrollment Process: Can I Enroll In Health Insurance Outside Of Open Enrollment
- Factors Influencing Enrollment Decisions
- Last Recap
- FAQ Section
Can I enroll in health insurance outside of open enrollment sets the stage for this enthralling narrative, offering readers a glimpse into a world where health insurance options extend beyond the traditional open enrollment periods. This exploration delves into the intricacies of special enrollment periods, the potential for enrolling outside of these designated times, and the consequences that may accompany such decisions.
Navigating the health insurance landscape can be complex, especially when it comes to understanding the nuances of enrollment periods. While open enrollment periods provide a designated window for individuals to select or change their health insurance plans, there are instances where enrollment outside of these periods might be possible. This guide aims to shed light on the various scenarios that allow for enrollment outside of open enrollment, the potential implications, and the steps involved in successfully navigating the process.
Understanding Open Enrollment Periods

Open enrollment periods are specific times of year when you can sign up for or change your health insurance plan without facing penalties for doing so outside of the designated timeframe. These periods are crucial for ensuring you have health coverage and making informed decisions about your insurance needs.
Duration and Significance of Open Enrollment Periods
Open enrollment periods are typically a few weeks long, and they vary depending on the type of health insurance plan. The significance of these periods lies in their ability to provide individuals and families with the opportunity to:
- Enroll in a health insurance plan for the first time.
- Switch to a different health insurance plan.
- Make changes to their existing health insurance plan.
Open Enrollment Periods for Different Health Insurance Plans
Here are some examples of open enrollment periods for different types of health insurance plans:
- Individual Health Insurance Plans: The open enrollment period for individual health insurance plans is typically from November 1st to January 15th. This period allows individuals to shop for and enroll in plans for the following calendar year.
- Employer-Sponsored Health Insurance Plans: Open enrollment periods for employer-sponsored health insurance plans are typically set by the employer and can vary. However, they are usually in the fall, allowing employees to choose their health insurance plans for the next calendar year.
- Medicare: The open enrollment period for Medicare is from October 15th to December 7th. This period allows Medicare beneficiaries to make changes to their Medicare coverage for the following year.
Special Enrollment Periods
Special enrollment periods (SEPs) are specific times outside of the annual open enrollment period when you can enroll in or change your health insurance plan. These periods are designed to allow individuals and families to make changes to their coverage when they experience certain life events that affect their health insurance needs.
Qualifying Life Events
These events trigger a special enrollment period, allowing you to enroll in or change your health insurance plan outside the annual open enrollment period.
- Loss of Coverage: Losing your health insurance due to job loss, divorce, or other reasons.
- Gaining Coverage: Getting married, having a baby, adopting a child, or gaining coverage through a spouse’s employer.
- Moving: Moving to a new geographic area where your previous health insurance plan is not available.
- Changes in Family Size: Getting married, having a baby, adopting a child, or experiencing a divorce.
- Changes in Income: Experiencing a significant change in income, such as a job loss or a reduction in work hours.
- Changes in Health Status: Being diagnosed with a serious health condition or having a significant change in your health status.
- Other Qualifying Life Events: The Affordable Care Act (ACA) Artikels other specific events that qualify for a SEP, including becoming a U.S. citizen or national, experiencing domestic violence, or being a victim of a natural disaster.
Eligibility Criteria and Documentation Requirements
To qualify for a special enrollment period, you must meet specific eligibility criteria and provide supporting documentation.
- Loss of Coverage: You must provide proof of your previous coverage, such as a termination notice or a cancellation letter from your previous insurer.
- Gaining Coverage: You must provide proof of the life event, such as a marriage certificate, birth certificate, adoption papers, or a letter from your spouse’s employer.
- Moving: You must provide proof of your new address, such as a utility bill or a lease agreement.
- Changes in Family Size: You must provide proof of the life event, such as a marriage certificate, birth certificate, adoption papers, or a divorce decree.
- Changes in Income: You must provide proof of your income change, such as a pay stub, tax return, or unemployment benefits statement.
- Changes in Health Status: You must provide documentation from your doctor or healthcare provider confirming the diagnosis or change in health status.
- Other Qualifying Life Events: You must provide documentation supporting the qualifying life event, such as a natural disaster declaration, a court order for domestic violence, or a U.S. citizenship or nationalization certificate.
Enrollment Outside of Open Enrollment
While open enrollment periods are the typical time to sign up for health insurance, there are situations where you might be able to enroll outside of these periods. These situations are known as special enrollment periods, and they allow you to enroll in a health insurance plan if you experience a qualifying life event.
Special Enrollment Periods
Special enrollment periods offer a window of opportunity to enroll in a health insurance plan outside of the regular open enrollment period. These periods are triggered by specific life events that significantly impact your health insurance needs.
- Loss of Employer-Sponsored Coverage: If you lose your job or your employer stops offering health insurance, you may be eligible for a special enrollment period to enroll in an individual health insurance plan.
- Marriage or Divorce: Getting married or divorced can change your health insurance needs. You may be eligible for a special enrollment period to add your spouse to your plan or to enroll in a new plan.
- Birth or Adoption: Welcoming a new child into your family is a significant life event that qualifies you for a special enrollment period. You can enroll your child in a health insurance plan.
- Moving to a New State: When you move to a new state, you may need to change your health insurance plan. This is another qualifying life event that allows you to enroll in a new plan outside of open enrollment.
- Changes in Household Size: If you experience a change in household size, such as a dependent leaving your household, you may be eligible for a special enrollment period.
- Changes in Income: Significant changes in your income can affect your eligibility for certain health insurance plans. If you lose your job or experience a significant income decrease, you may qualify for a special enrollment period.
- Changes in Coverage: If you are enrolled in a health insurance plan that is no longer offered or if your plan changes significantly, you may be eligible for a special enrollment period to switch to a different plan.
Types of Health Insurance Plans
Several types of health insurance plans may offer enrollment outside of open enrollment periods:
- Individual Health Insurance Plans: These plans are purchased directly from an insurance company, and they are often available through the Health Insurance Marketplace. Many individual plans allow enrollment outside of open enrollment periods due to qualifying life events.
- Short-Term Health Insurance Plans: Short-term plans are typically offered for a limited duration, often for a few months or a year. They may be available outside of open enrollment periods but usually have limited coverage compared to traditional health insurance plans.
Consequences of Enrollment Outside Open Enrollment

Enrolling in health insurance outside of open enrollment periods might seem convenient, but it often comes with certain downsides. These consequences can vary depending on your circumstances and the specific insurance plan you choose.
Higher Premiums, Can i enroll in health insurance outside of open enrollment
Enrolling outside of open enrollment might mean you’ll pay a higher premium than you would have during the regular enrollment period. Insurance companies typically offer lower premiums during open enrollment as a way to attract new customers. Outside of this period, they might offer limited plan options, and the premiums for these plans could be significantly higher.
Limited Plan Options
You might not have as many plan options available outside of open enrollment as you would during the regular period. This is because insurance companies often limit the number of plans they offer outside of open enrollment. This means you might not be able to find a plan that perfectly fits your needs and budget.
Penalties
In some cases, you might face penalties for enrolling in health insurance outside of open enrollment. For instance, if you are enrolling in a plan through the Affordable Care Act marketplace, you might be required to pay a penalty if you don’t have health insurance for a certain period. This penalty is usually calculated based on your income and the length of time you were uninsured.
Navigating the Enrollment Process: Can I Enroll In Health Insurance Outside Of Open Enrollment
Enrolling in health insurance outside of open enrollment can seem daunting, but it’s achievable with the right information and steps. This section will provide a comprehensive guide to navigate the enrollment process, outlining the essential steps, required documentation, and the importance of seeking support from insurance providers.
Steps to Enroll in Health Insurance Outside Open Enrollment
Enrolling in health insurance outside of open enrollment requires a qualifying event. These events trigger a special enrollment period, allowing you to enroll in a new health plan. The following steps Artikel the enrollment process:
- Identify a Qualifying Event: The first step is to determine if you have experienced a qualifying event. These events include life changes such as getting married, having a baby, losing health insurance coverage, or moving to a new state. A comprehensive list of qualifying events is available on the official website of the Health Insurance Marketplace.
- Gather Required Documentation: Once you have identified a qualifying event, gather the necessary documentation to support your application. This documentation may include your marriage certificate, birth certificate, proof of job loss, or proof of address change. The specific documents required will vary depending on your qualifying event.
- Contact an Insurance Provider: After gathering the required documentation, contact an insurance provider to initiate the enrollment process. You can reach out to an insurance provider directly or through the Health Insurance Marketplace. The insurance provider will guide you through the enrollment process and answer any questions you may have.
- Complete the Application: The insurance provider will provide you with an application to complete. The application will require information about your personal details, employment status, income, and health history. It is essential to provide accurate and complete information to ensure a smooth enrollment process.
- Review and Submit the Application: After completing the application, review it carefully to ensure all information is correct. Once you are satisfied with the information, submit the application to the insurance provider. The insurance provider will review your application and process your enrollment.
Essential Information and Documentation for Enrollment
To ensure a smooth enrollment process, it’s crucial to have the necessary information and documentation readily available. Here’s a list of essential items:
- Proof of Identity: This could include a driver’s license, passport, or social security card.
- Proof of Citizenship or Legal Residency: This could include a birth certificate, naturalization certificate, or green card.
- Proof of Income: This could include tax returns, pay stubs, or bank statements.
- Proof of Address: This could include a utility bill, bank statement, or lease agreement.
- Proof of Qualifying Event: This could include a marriage certificate, birth certificate, job loss notice, or proof of address change.
- Health Information: This may include details about your health conditions, medications, and previous medical treatments. Sharing this information is important for the insurance provider to assess your health and determine the appropriate plan for your needs.
Contacting Insurance Providers for Guidance and Support
Navigating the enrollment process can be overwhelming, especially when dealing with complex insurance terms and procedures. It is highly recommended to contact insurance providers for guidance and support. They can provide personalized assistance, answer questions, and clarify any doubts you may have. Here are some reasons why contacting insurance providers is essential:
- Expert Guidance: Insurance providers have extensive knowledge about health insurance plans and enrollment processes. They can guide you through the steps, explain the different plan options, and help you choose the most suitable plan for your needs and budget.
- Personalized Assistance: Each individual’s circumstances are unique, and insurance providers can offer personalized assistance based on your specific needs. They can help you understand the different coverage options, determine the best plan for your health conditions, and answer any questions you may have.
- Resolution of Queries: Insurance providers are equipped to handle inquiries and resolve any issues that may arise during the enrollment process. They can provide clarification on specific plan details, address concerns about eligibility, and assist with any technical difficulties you may encounter.
- Support and Resources: Insurance providers can offer additional support and resources to ensure a smooth enrollment experience. They may have online tools, brochures, or other materials that can help you understand the process and make informed decisions.
Factors Influencing Enrollment Decisions
Deciding whether to enroll in health insurance outside of open enrollment is a significant decision that requires careful consideration of various factors. These factors can be categorized into personal needs, health status, financial situation, and potential consequences of delaying enrollment.
Individual Needs and Health Status
Understanding your individual needs and health status is crucial in determining the necessity of enrolling in health insurance outside of open enrollment. Your health history, current health conditions, and potential future health needs all play a role in this decision.
- If you have a pre-existing condition, you may want to enroll in health insurance as soon as possible to avoid potential coverage gaps and high out-of-pocket costs.
- If you are expecting a child or planning a major medical procedure, you may need to enroll in health insurance to ensure coverage for these events.
- If you are healthy and have a low risk of needing medical care, you may be able to wait until the next open enrollment period to enroll.
Financial Situation
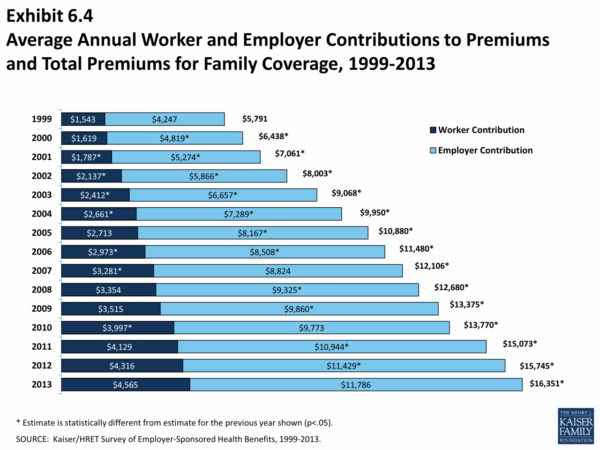
Your financial situation is another important factor to consider. Health insurance premiums, deductibles, and co-pays can vary widely depending on the plan you choose.
- If you have a limited budget, you may want to compare different plans to find one that fits your financial needs.
- You may also want to consider the potential financial impact of not having health insurance, such as the cost of unexpected medical bills.
Coverage Gaps and Potential Penalties
Enrolling in health insurance outside of open enrollment can result in coverage gaps, which can leave you vulnerable to high medical costs. You may also be subject to penalties for not having health insurance.
- If you are enrolled in a health insurance plan, you may be subject to a penalty if you let your coverage lapse.
- You may also be subject to a penalty if you do not have health insurance and you are required to have it by law.
Last Recap

Understanding the intricacies of health insurance enrollment, including the possibilities of enrolling outside of open enrollment periods, is crucial for making informed decisions about your health coverage. By carefully considering your individual circumstances, exploring the available options, and seeking guidance from insurance providers, you can navigate the enrollment process with confidence and ensure that you have the right health insurance plan to meet your needs.
FAQ Section
What are the common reasons for special enrollment periods?
Special enrollment periods are typically triggered by significant life events, such as getting married, having a baby, losing health insurance coverage, or moving to a new state.
Can I enroll in a different health insurance plan outside of open enrollment?
While you may not be able to enroll in a completely different health insurance plan outside of open enrollment, you might be able to make changes to your existing plan, such as adding a dependent or switching to a different coverage level.
What are the potential penalties for enrolling outside of open enrollment?
The penalties for enrolling outside of open enrollment can vary depending on the circumstances. You may face higher premiums, limited plan options, or even a denial of coverage altogether.
What documentation do I need to enroll in health insurance outside of open enrollment?
The specific documentation required will depend on the reason for enrolling outside of open enrollment. You may need to provide proof of a life event, such as a marriage certificate or a birth certificate, or documentation related to a change in your employment status.