- Understanding Qualifying Events
- Circumstances Allowing Enrollment Without Qualifying Events
- Special Enrollment Periods
- State-Specific Regulations
- Impact of Health Insurance Marketplace
- Alternative Insurance Options
- Potential Consequences of Enrollment Without Qualifying Events
- Tips for Navigating Enrollment Processes: Can I Get Health Insurance Without A Qualifying Event
- Ending Remarks
- FAQ Insights
Can I get health insurance without a qualifying event? It’s a question many individuals ask, especially those who haven’t experienced a life-changing event like marriage, birth, or job loss. The truth is, obtaining health insurance outside of open enrollment periods can be tricky, but not impossible. There are specific circumstances and regulations that dictate eligibility for enrollment, and understanding them is crucial.
This article delves into the complexities of obtaining health insurance without a qualifying event, exploring the various scenarios, regulations, and alternative options available. We’ll examine the role of qualifying events, special enrollment periods, and the impact of the Health Insurance Marketplace on enrollment options. We’ll also discuss potential consequences of enrolling without a qualifying event and provide practical tips for navigating the enrollment process.
Understanding Qualifying Events
Qualifying events are specific life changes that allow individuals to enroll in health insurance outside of the annual open enrollment period. These events are designed to ensure that individuals have access to health insurance when they need it most, even if they miss the open enrollment window.
Examples of Qualifying Events
Qualifying events are defined by the Affordable Care Act (ACA) and can vary slightly depending on the state. Some common qualifying events include:
- Loss of Job-Based Coverage: If you lose your job or your employer stops offering health insurance, you may be eligible to enroll in a health insurance plan outside of open enrollment.
- Marriage or Divorce: Getting married or divorced can trigger a qualifying event, allowing you to enroll in a new health insurance plan that reflects your new family status.
- Birth or Adoption of a Child: Welcoming a new child into your family is a qualifying event that allows you to enroll in a health insurance plan that covers your growing family.
- Moving to a New State: If you relocate to a new state, you may be eligible to enroll in a health insurance plan that is available in your new location.
- Turning 26 Years Old: When you turn 26, you are no longer eligible to be covered under your parents’ health insurance plan. This is a qualifying event that allows you to enroll in your own health insurance plan.
Rationale Behind Qualifying Events
The rationale behind requiring qualifying events for enrollment is to balance the need for access to health insurance with the need for a stable and predictable health insurance market. By limiting enrollment to specific events, insurers can better manage their risk and ensure that premiums remain affordable for everyone.
Circumstances Allowing Enrollment Without Qualifying Events
While qualifying events typically trigger open enrollment periods for health insurance, there are specific situations where individuals may be eligible to enroll outside these periods. These situations are often designed to address unique circumstances and ensure access to healthcare for those who might otherwise be excluded.
Special Enrollment Periods, Can i get health insurance without a qualifying event
Special enrollment periods offer opportunities to enroll in health insurance outside of the regular open enrollment period. These periods are triggered by specific life events, such as:
- Loss of other health coverage: If you lose your job-based health insurance or coverage through a family member, you may be eligible for a special enrollment period.
- Moving to a new coverage area: If you relocate to a new geographic area, you may be eligible for a special enrollment period to find new coverage in your new location.
- Marriage or divorce: Significant life changes like marriage or divorce can affect your health insurance needs and may trigger a special enrollment period.
- Birth or adoption of a child: Welcoming a new family member can create a need for additional health insurance coverage, allowing for a special enrollment period.
- Changes in household income: If you experience a significant increase or decrease in your household income, you may be eligible for a special enrollment period to adjust your health insurance plan.
Medicaid Eligibility
Medicaid is a government-funded health insurance program for low-income individuals and families. Eligibility for Medicaid varies by state, but generally includes factors such as:
- Income: Your income must fall below a certain threshold to qualify for Medicaid.
- Family size: The number of individuals in your household influences your eligibility.
- Citizenship status: You must be a U.S. citizen or a qualified non-citizen to be eligible.
- Disability: Individuals with disabilities may qualify for Medicaid, even if their income exceeds the standard threshold.
Marketplace Eligibility
The Affordable Care Act’s Health Insurance Marketplace offers individuals and families access to health insurance plans, including subsidies to help offset costs. Eligibility for Marketplace plans is based on:
- Income: You must meet certain income requirements to qualify for subsidies.
- Citizenship status: You must be a U.S. citizen or a qualified non-citizen to be eligible.
- Residency: You must reside in a state that participates in the Marketplace.
Special Enrollment Periods
Special enrollment periods (SEPs) are timeframes outside of the annual open enrollment period when you can enroll in or change your health insurance plan. Unlike open enrollment, which occurs once a year for a limited time, SEPs allow you to make changes to your health insurance coverage based on specific life events. These events can be significant changes in your personal circumstances, such as getting married, having a baby, or losing your job.
Events That Trigger Special Enrollment Periods
SEPs are designed to ensure that individuals have access to health insurance when they need it, even if they miss the open enrollment period. These periods allow people to enroll in or change their health insurance plans without facing penalties for late enrollment.
- Loss of Job-Based Coverage: If you lose your job-based health insurance coverage, you have 60 days from the date of your job loss to enroll in a new health insurance plan through the Marketplace.
- Marriage or Divorce: If you get married or divorced, you have 60 days from the date of the event to enroll in a new health insurance plan or change your existing coverage.
- Birth or Adoption of a Child: You have 60 days from the date of birth or adoption to enroll in a new health insurance plan or add your child to your existing coverage.
- Moving to a New Coverage Area: If you move to a new coverage area, you may have 60 days to enroll in a new health insurance plan.
- Loss of Coverage Due to a Change in Employer: If your employer changes your health insurance plan, you may have 60 days to enroll in a new plan through the Marketplace.
- Becoming Eligible for Medicaid or CHIP: If you become eligible for Medicaid or CHIP, you can enroll in these programs at any time.
- Certain Life Events: Other life events, such as becoming a U.S. citizen, becoming a lawful permanent resident, or losing your health insurance due to a change in your coverage, may also qualify you for a SEP.
Timeframe for Enrolling During Special Enrollment Periods
You typically have 60 days from the date of the qualifying event to enroll in a new health insurance plan or make changes to your existing coverage. However, it’s important to note that the specific timeframe may vary depending on the qualifying event and the state you live in. It’s always best to check with the Marketplace or your health insurance provider to confirm the exact timeframe for your situation.
State-Specific Regulations

While federal regulations set the foundation for health insurance enrollment, states have the authority to implement their own rules and programs that can affect your ability to enroll outside of a qualifying event. Understanding these state-specific regulations is crucial for navigating the health insurance landscape and accessing the best options available.
State-Specific Programs and Policies
Many states have established programs and policies that offer alternative enrollment options beyond the traditional qualifying events. These programs aim to provide access to health insurance for individuals who may not qualify for enrollment through the federal marketplace or through their employer.
- State-Based Marketplaces: Some states have their own marketplaces, which may have different rules and eligibility requirements than the federal marketplace. For example, certain states may offer extended enrollment periods or provide subsidies for individuals with specific income levels.
- State-Specific Programs: Several states have implemented programs that offer subsidized health insurance to low-income individuals or those with specific health conditions. These programs may have their own eligibility requirements and enrollment periods.
- Special Enrollment Periods: Some states have extended special enrollment periods beyond the federal guidelines, allowing individuals to enroll in health insurance due to certain life events, such as marriage, divorce, or the birth of a child.
Understanding State Regulations
To ensure you have access to all available enrollment options, it is crucial to understand the specific regulations in your state. Here are some steps you can take to gather this information:
- Visit Your State’s Health Insurance Marketplace Website: Each state’s marketplace website will provide detailed information about enrollment options, eligibility requirements, and special enrollment periods.
- Contact Your State’s Department of Insurance: The state’s Department of Insurance can provide additional information about state-specific programs and regulations.
- Consult with a Licensed Insurance Agent: A licensed insurance agent can help you navigate the complexities of state regulations and find the best health insurance options for your situation.
Remember, state regulations can vary significantly, so it’s essential to research and understand the rules in your specific location. This will help you make informed decisions about your health insurance coverage and ensure you have access to the best options available.
Impact of Health Insurance Marketplace
The Health Insurance Marketplace, also known as the Affordable Care Act (ACA) Marketplace, significantly impacts enrollment options for health insurance. It provides a platform for individuals and families to compare and purchase health insurance plans from various private insurance companies.
Enrollment Options Through the Marketplace
The Marketplace offers various enrollment options, including:
- Open Enrollment Period: This annual period typically runs from November 1st to January 15th, during which individuals can enroll in or change their health insurance plans.
- Special Enrollment Period: Individuals may qualify for a Special Enrollment Period if they experience a qualifying life event, such as getting married, having a baby, losing job-based coverage, or moving to a new state. These periods allow individuals to enroll outside the open enrollment period.
Plans Available Outside of Open Enrollment Periods
The Marketplace allows individuals to enroll in or change their health insurance plans outside of the open enrollment period if they experience a qualifying life event. This includes:
- Loss of Job-Based Coverage: If you lose your job-based health insurance due to job loss or a change in employment status, you can enroll in a Marketplace plan within 60 days of losing your coverage.
- Moving to a New State: If you move to a new state, you can enroll in a Marketplace plan within 60 days of moving.
- Marriage or Divorce: If you get married or divorced, you can enroll in a Marketplace plan within 60 days of the event.
- Birth or Adoption of a Child: If you have a baby or adopt a child, you can enroll in a Marketplace plan within 60 days of the event.
- Changes in Household Income: If your household income changes significantly, you may be eligible for a Special Enrollment Period to change your plan.
Marketplace vs. Private Insurers
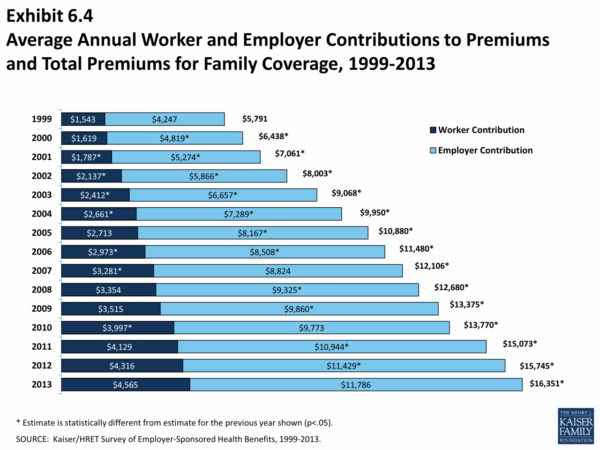
The Marketplace and private insurers offer different enrollment options and plan choices. Here’s a comparison:
| Feature | Marketplace | Private Insurers |
|---|---|---|
| Enrollment Periods | Open Enrollment, Special Enrollment Periods | Open Enrollment, Special Enrollment Periods, may offer other enrollment periods based on their policies |
| Plan Availability | Wide range of plans from various insurance companies | May offer a limited range of plans |
| Financial Assistance | Tax credits and subsidies based on income | May offer discounts or programs, but not as extensive as Marketplace assistance |
| Eligibility | Open to most individuals and families | Eligibility varies based on insurer policies |
Alternative Insurance Options
If you’re unable to enroll in traditional health insurance due to the lack of a qualifying event, there are alternative insurance options available that can provide some level of coverage. These options often come with different coverage levels, limitations, and costs compared to traditional health insurance.
Short-Term Health Insurance
Short-term health insurance is a temporary coverage option that typically lasts for a few months. It’s often used as a stopgap measure while waiting for a qualifying event or during a period of unemployment. Short-term plans generally have lower premiums than traditional health insurance, but they also have limited coverage.
- Coverage: Short-term plans typically cover essential medical services like hospital stays, surgery, and emergency care. However, they often exclude coverage for pre-existing conditions, preventive care, and mental health services.
- Limitations: Short-term plans are not designed for long-term coverage. They may have a maximum coverage period, and you may need to reapply for coverage after the initial term. The premiums can also increase significantly if you need to renew the plan.
- Benefits: Short-term plans can be a good option for individuals who need temporary coverage and are healthy. They are also generally less expensive than traditional health insurance plans.
- Drawbacks: Short-term plans have limited coverage and may not be suitable for individuals with pre-existing conditions or those who need comprehensive health insurance.
Health Sharing Ministries
Health sharing ministries are faith-based organizations that operate on a sharing model. Members contribute to a common fund that is used to pay for medical expenses. These ministries typically have lower costs than traditional health insurance, but they also have limitations.
- Coverage: Health sharing ministries typically cover a wide range of medical expenses, including hospital stays, surgery, and doctor’s visits. However, they may have restrictions on coverage for certain conditions or treatments, and they may not cover preventive care.
- Limitations: Health sharing ministries are not considered insurance, and they are not regulated by state insurance departments. This means that they may not provide the same level of consumer protection as traditional health insurance plans. Additionally, membership in a health sharing ministry is typically based on religious beliefs, which may not be suitable for everyone.
- Benefits: Health sharing ministries can be a cost-effective option for individuals who are seeking affordable healthcare and who are comfortable with their religious requirements. They often have a strong sense of community and support among their members.
- Drawbacks: Health sharing ministries may not cover all medical expenses, and they may not provide the same level of consumer protection as traditional health insurance plans. Membership is often based on religious beliefs, which may not be suitable for everyone.
Direct Primary Care
Direct primary care (DPC) is a healthcare model that offers patients unlimited access to their primary care physician for a monthly fee. This model can be a good option for individuals who are looking for affordable, personalized care.
- Coverage: DPC typically covers preventive care, routine checkups, and basic medical services. However, it does not usually cover hospital stays, surgery, or other expensive medical procedures.
- Limitations: DPC is not a replacement for traditional health insurance. You will still need health insurance to cover major medical expenses. Additionally, DPC may not be available in all areas.
- Benefits: DPC can be a cost-effective option for individuals who are healthy and need basic medical care. It can also provide patients with greater access to their primary care physician.
- Drawbacks: DPC does not cover major medical expenses, and it may not be available in all areas. It may also not be suitable for individuals with complex medical needs.
Potential Consequences of Enrollment Without Qualifying Events
Enrolling in health insurance without a qualifying event can have serious consequences. These consequences are designed to ensure that people only enroll when they are truly eligible, and to prevent people from gaming the system by enrolling only when they need healthcare. This helps to keep healthcare costs manageable for everyone.
Penalties and Fines
Individuals who enroll in health insurance without a qualifying event may face penalties or fines. These penalties can vary depending on the specific circumstances and the state or federal regulations in place. It is important to note that these penalties can be substantial and may impact your financial well-being.
- Late Enrollment Penalty: This penalty can apply if you enroll in health insurance outside of the open enrollment period without a qualifying event. The penalty is typically calculated as a percentage of your annual premium, and it can be quite significant.
- Individual Shared Responsibility Payment: This penalty was part of the Affordable Care Act (ACA) and applied to individuals who did not have health insurance. It was eliminated in 2019. However, some states have implemented their own individual mandates with penalties.
- Denial of Coverage: In some cases, your insurance company may deny your application for coverage if they determine that you did not have a qualifying event. This can leave you without health insurance and potentially facing significant medical expenses.
Importance of Adhering to Enrollment Regulations
It is crucial to understand and adhere to the enrollment regulations for health insurance. Failing to do so can result in serious consequences, including financial penalties and denial of coverage. It is always best to consult with an insurance professional or refer to the official guidelines of your state or the federal government to ensure you are following the correct procedures for enrollment.
Tips for Navigating Enrollment Processes: Can I Get Health Insurance Without A Qualifying Event

Navigating the health insurance enrollment process can be complex, but with the right knowledge and resources, you can make the process smoother. Here are some practical tips to guide you through the enrollment process.
Utilize Available Resources
The enrollment process can be overwhelming, but there are several resources available to assist you.
- Health Insurance Marketplace Website: The Health Insurance Marketplace website provides comprehensive information on plans, eligibility requirements, and enrollment procedures. You can access the website through Healthcare.gov.
- State-Specific Resources: Each state has its own resources and support services for health insurance enrollment. Contact your state’s health insurance marketplace or department of insurance for assistance.
- Insurance Navigators: Insurance navigators are trained professionals who provide free, unbiased guidance on health insurance options. They can help you understand your coverage options, compare plans, and complete the enrollment process. You can find a navigator in your area through the Health Insurance Marketplace website.
- Consumer Assistance Programs: Various organizations offer consumer assistance programs that can provide support and guidance during the enrollment process. These programs often provide free counseling, plan comparisons, and enrollment assistance. Contact your local community center or social service agency to inquire about available programs.
Gather Necessary Information
Before starting the enrollment process, gather all necessary information to ensure a smooth experience.
- Social Security Number: Your Social Security number is essential for verifying your identity and eligibility for health insurance plans.
- Income Information: You will need to provide income information, including tax returns and pay stubs, to determine your eligibility for subsidies and tax credits.
- Family Information: If you are enrolling for your family, you will need to provide information about your dependents, including their Social Security numbers and birthdates.
- Current Insurance Information: If you have existing health insurance, gather your policy details, including your policy number and coverage details.
Plan Ahead and Set Deadlines
Planning ahead and setting deadlines can help you avoid last-minute rushes and potential penalties.
- Open Enrollment Period: The open enrollment period for health insurance plans typically runs from November 1st to January 15th. During this period, you can enroll in or change health insurance plans without a qualifying event.
- Special Enrollment Periods: If you experience a qualifying event, you may be eligible for a special enrollment period, allowing you to enroll outside of the open enrollment period. Common qualifying events include losing your job, getting married, or having a baby.
- Plan Deadlines: Be aware of the deadlines for submitting your application and paying your premiums. Late submissions or payments may result in penalties or coverage gaps.
Compare Plans Thoroughly
Compare different plans to find the best option for your needs and budget.
- Plan Benefits: Consider the coverage provided by each plan, including deductibles, copayments, and out-of-pocket maximums. Make sure the plan covers the services you need.
- Network Coverage: Ensure that your preferred doctors and hospitals are included in the plan’s network. Out-of-network care can be significantly more expensive.
- Prescription Drug Coverage: If you take prescription medications, check the plan’s formulary to see if your medications are covered and what the copayments are.
- Premium Costs: Compare the monthly premiums of different plans. Consider your budget and the value of the coverage offered by each plan.
Review Your Enrollment Information
Carefully review all information before submitting your enrollment application.
- Accuracy of Information: Double-check that all your personal and financial information is accurate and complete. Errors can lead to delays or denials of coverage.
- Plan Details: Verify the details of the plan you are enrolling in, including coverage benefits, network providers, and premium costs.
- Enrollment Confirmation: Once you submit your application, you will receive an enrollment confirmation. Review this confirmation carefully to ensure you have the correct plan and coverage.
Seek Assistance When Needed
If you encounter any difficulties during the enrollment process, don’t hesitate to seek assistance.
- Contact Customer Support: The Health Insurance Marketplace website and insurance companies have customer support teams that can answer your questions and provide assistance.
- Reach Out to Navigators: Insurance navigators are available to help you navigate the enrollment process and address any concerns you may have.
- Consult with a Broker: If you need personalized guidance, consider consulting with a health insurance broker. Brokers can help you compare plans and find the best option for your needs.
Understand Your Coverage
Once you are enrolled in a health insurance plan, it’s crucial to understand your coverage.
- Policy Documents: Review your policy documents carefully to understand your benefits, coverage limits, and out-of-pocket expenses.
- Explanation of Benefits: When you receive medical care, you will receive an explanation of benefits (EOB) outlining the costs associated with your care and the amount your insurance paid.
- Customer Service: Contact your insurance company’s customer service if you have any questions about your coverage or claims.
Ending Remarks
Navigating the world of health insurance can be a daunting task, especially when it comes to understanding the intricacies of qualifying events and enrollment periods. While enrolling without a qualifying event might seem challenging, it’s not entirely impossible. By understanding the various options available, researching state-specific regulations, and seeking professional guidance, individuals can increase their chances of securing the health insurance coverage they need.
FAQ Insights
Can I get health insurance if I’m self-employed?
Yes, you can usually obtain health insurance if you’re self-employed. You can explore individual health insurance plans through the Health Insurance Marketplace or directly from private insurers.
What are the penalties for enrolling in health insurance without a qualifying event?
The penalties for enrolling without a qualifying event vary depending on your situation and the specific state regulations. It’s best to consult with an insurance professional or review your state’s health insurance website for detailed information.
Are there any special enrollment periods for students?
Yes, students may be eligible for special enrollment periods if they lose their student health insurance coverage, experience a change in their student status, or if their income falls below a certain threshold.