When Were HIV Laws Created sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. The emergence of HIV/AIDS as a global health crisis in the early 1980s sparked a whirlwind of fear, misinformation, and a desperate need for understanding. This period saw a rapid evolution of scientific knowledge about the virus, coupled with societal reactions that ranged from compassion to prejudice. As the epidemic spread, governments around the world grappled with the challenge of responding effectively, leading to the creation of a complex web of laws designed to manage the virus, protect individuals, and prevent further transmission.
This journey through the history of HIV laws reveals a tapestry woven with threads of science, public health, human rights, and social justice. It explores the initial responses to the epidemic, the evolution of legal frameworks, and the impact these laws have had on individuals, communities, and public health outcomes. It delves into the complexities of HIV testing, disclosure, and confidentiality, as well as the legal protections afforded to people living with HIV. The narrative also examines the controversial issue of criminalizing HIV exposure, analyzing its implications and potential unintended consequences.
Historical Context: When Were Hiv Laws Created
The emergence of HIV/AIDS as a global health crisis in the late 20th century had a profound impact on societies worldwide. The disease’s rapid spread, coupled with limited understanding and treatment options, fueled fear, stigma, and discrimination. This section explores the historical context of HIV/AIDS, examining its initial understanding, scientific knowledge, and societal responses.
Initial Understanding and Scientific Knowledge
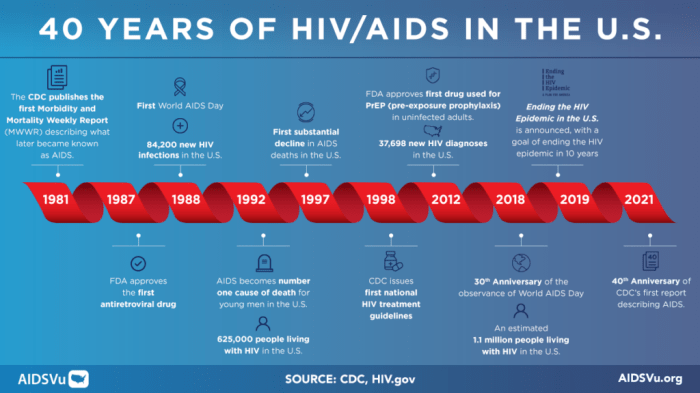
The early understanding of HIV/AIDS was marked by confusion and uncertainty. In the early 1980s, a cluster of unusual pneumonia cases and rare cancers among gay men in the United States raised concerns about a new and unknown disease. Initial research focused on identifying the cause and transmission routes. The discovery of the human immunodeficiency virus (HIV) in 1983 marked a significant breakthrough, but the initial understanding of its mechanisms and the potential for treatment was limited.
Early research revealed that HIV attacks the immune system, leaving individuals vulnerable to opportunistic infections. The virus’s ability to mutate and develop resistance to treatment posed significant challenges for scientists and clinicians.
Early Public Reactions and Societal Responses
The emergence of HIV/AIDS was met with widespread fear and prejudice. The disease was initially associated with specific populations, including gay men, intravenous drug users, and people of color, leading to social stigma and discrimination.
“The AIDS epidemic was not just a medical crisis; it was a social crisis as well.” – Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases
The initial public response to the epidemic was characterized by fear, misinformation, and lack of understanding. Some individuals and communities engaged in discriminatory practices, such as refusing to share needles with people who injected drugs or isolating individuals with HIV/AIDS.
The lack of effective treatment options further fueled anxiety and desperation. The fear of transmission led to social isolation and the marginalization of individuals with HIV/AIDS.
The early societal responses to HIV/AIDS were often marked by prejudice and misinformation. These responses highlight the importance of education, empathy, and understanding in addressing public health crises.
Legal Responses and Legislation
The global response to HIV/AIDS has been shaped by a complex interplay of scientific, social, and legal factors. The emergence of the virus prompted governments worldwide to grapple with the challenges of public health, human rights, and social stigma. This section explores the evolution of legal responses to HIV/AIDS, examining the early legislation, the diverse approaches across regions, and the ongoing efforts to ensure that laws are both effective and humane.
Early Legal Responses, When were hiv laws created
Early legal responses to HIV/AIDS were often driven by fear and misinformation. Many countries implemented measures that focused on isolation, quarantine, and criminalization, reflecting a lack of understanding about the virus and its transmission. For instance, in the United States, the Centers for Disease Control and Prevention (CDC) issued guidelines in 1987 that recommended mandatory HIV testing for certain groups, including healthcare workers, and the reporting of positive test results to public health authorities. Similarly, in the United Kingdom, the Public Health (Control of Diseases) Act 1984 granted the government powers to detain individuals with HIV/AIDS, although these powers were rarely used.
Comparative Approaches to Legal Regulation
The legal regulation of HIV/AIDS has varied significantly across different regions, reflecting diverse cultural, political, and legal contexts. In some countries, a human rights-based approach has prevailed, emphasizing the importance of informed consent, confidentiality, and non-discrimination. For example, in Canada, the Canadian Charter of Rights and Freedoms guarantees the right to privacy and prohibits discrimination on the basis of health status. In contrast, other countries have adopted more restrictive legal frameworks, often influenced by moral and religious beliefs. In some African countries, for example, laws criminalizing same-sex relationships have been used to target and stigmatize individuals living with HIV/AIDS.
Evolution of HIV/AIDS Laws
Over time, HIV/AIDS laws have evolved in response to growing scientific knowledge, changing social attitudes, and advocacy efforts. One significant development has been the shift away from mandatory HIV testing and towards voluntary testing and counseling. Many countries have also introduced legislation to protect the rights of individuals living with HIV/AIDS, including the right to confidentiality, access to healthcare, and non-discrimination in employment and education. Another important trend has been the decriminalization of HIV transmission, with many countries recognizing that criminalizing HIV exposure or transmission is ineffective and counterproductive. For example, in the United States, the Centers for Disease Control and Prevention (CDC) issued guidelines in 2016 that recommended against criminalizing HIV exposure or transmission, arguing that such laws are often based on fear and misinformation and can deter individuals from seeking testing and treatment.
Key Issues Addressed by HIV Laws
HIV laws have been instrumental in shaping public health responses to the epidemic, addressing critical issues related to testing, disclosure, confidentiality, and discrimination. These laws aim to balance individual rights with public health concerns, while also protecting the rights of people living with HIV.
HIV Testing
HIV testing is a crucial component of public health strategies for HIV prevention and treatment. Laws governing HIV testing aim to ensure that individuals have access to accurate and confidential testing services while protecting their privacy and autonomy.
- Voluntary and Informed Consent: HIV testing should be voluntary and informed, meaning that individuals must be fully aware of the risks and benefits of testing before making a decision. This principle is enshrined in international human rights law and is reflected in many national laws.
- Confidentiality and Privacy: HIV test results are highly sensitive personal information, and laws protect the confidentiality of test results. This means that only authorized individuals, such as the person being tested or their healthcare provider, can access the results.
- Access to Testing: Laws should ensure that individuals have access to affordable and readily available HIV testing services, particularly in communities most affected by HIV. This includes providing testing services in healthcare settings, community-based organizations, and mobile clinics.
HIV Disclosure
HIV disclosure refers to the process of informing others about one’s HIV status. Laws governing HIV disclosure aim to strike a balance between protecting the privacy of people living with HIV and the need to prevent HIV transmission.
- Duty to Disclose: Some jurisdictions have laws that require individuals living with HIV to disclose their status to sexual partners or in other specific situations, such as before engaging in certain activities that pose a risk of transmission. These laws often focus on situations where there is a significant risk of transmission and where disclosure is necessary to protect the health of others.
- Exceptions to Disclosure: Laws may include exceptions to disclosure requirements, such as when disclosure would put the individual at risk of harm or when it is not feasible to disclose, for example, in situations of coercion or violence.
- Confidentiality and Privacy: Laws generally protect the confidentiality of HIV status, meaning that individuals are not required to disclose their status to anyone unless there is a legal obligation to do so.
Confidentiality and Privacy
Confidentiality and privacy are fundamental rights that are essential for protecting the well-being of people living with HIV. Laws addressing confidentiality and privacy aim to ensure that HIV-related information is kept confidential and that individuals are protected from discrimination and stigma.
- Protection of Medical Records: Laws protect the confidentiality of medical records, including HIV-related information. This means that healthcare providers and other individuals who have access to these records are legally obligated to keep them confidential.
- Access to Information: Laws may also address the right of individuals to access their own medical records, including HIV-related information. This right is important for individuals to understand their health status and make informed decisions about their healthcare.
- Restrictions on Disclosure: Laws often restrict the disclosure of HIV-related information to unauthorized individuals. This includes restrictions on the disclosure of information to employers, insurance companies, and other third parties.
Legal Protections for People Living with HIV
Laws play a crucial role in protecting the rights of people living with HIV from discrimination and stigma. Anti-discrimination laws are designed to ensure that individuals living with HIV are treated fairly and equally in all aspects of life.
- Employment: Laws protect individuals living with HIV from discrimination in employment, including hiring, promotion, and termination. This means that employers cannot discriminate against someone based on their HIV status.
- Housing: Laws protect individuals living with HIV from discrimination in housing, including rental and purchase of property. This means that landlords cannot discriminate against someone based on their HIV status.
- Education: Laws protect individuals living with HIV from discrimination in education, including access to schools, colleges, and universities. This means that educational institutions cannot discriminate against someone based on their HIV status.
- Healthcare: Laws protect individuals living with HIV from discrimination in healthcare, including access to medical care, treatment, and insurance. This means that healthcare providers and insurance companies cannot discriminate against someone based on their HIV status.
Legal Implications of HIV Transmission
The legal implications of HIV transmission are complex and vary widely across jurisdictions. Laws addressing HIV transmission aim to balance the need to protect public health with the rights of individuals living with HIV.
- Criminalization of HIV Exposure: Some jurisdictions have laws that criminalize HIV exposure, even if transmission does not occur. These laws often focus on situations where individuals with HIV engage in sexual activity without disclosing their status or taking steps to prevent transmission. However, these laws have been criticized for being discriminatory and for deterring people from seeking testing and treatment.
- Duty of Care: In some jurisdictions, laws may impose a duty of care on individuals living with HIV to take steps to prevent transmission. This duty may include disclosing their status to sexual partners, using condoms, and adhering to medical treatment.
- Consent and Disclosure: Laws generally require that sexual activity be consensual and that individuals are aware of the risks involved. This means that individuals living with HIV have a legal obligation to disclose their status to sexual partners before engaging in sexual activity.
Impact of HIV Laws on Individuals and Communities
HIV laws have had a profound impact on the lives of individuals living with HIV and the communities they belong to. These laws have shaped how people access healthcare, disclose their status, and interact with society. While some laws have aimed to protect public health, others have been criticized for their discriminatory and stigmatizing effects. This section will explore the diverse impacts of HIV laws on individuals and communities, examining both their potential benefits and drawbacks.
Impact on Individuals Living with HIV
HIV laws have significantly impacted individuals living with HIV in various ways, often leading to challenges and discrimination. For example, in some countries, mandatory HIV testing and disclosure laws have been implemented, forcing individuals to reveal their status against their will. This can lead to social stigma, discrimination, and even violence, making it difficult for individuals to access healthcare, maintain employment, or build relationships.
- Stigma and Discrimination: HIV laws that mandate disclosure or criminalize non-disclosure can create a climate of fear and stigma, leading to discrimination in employment, housing, and healthcare. Individuals may be reluctant to seek testing or treatment due to fear of being ostracized or facing legal consequences.
- Barriers to Healthcare Access: Mandatory HIV testing and reporting requirements can deter individuals from seeking testing and treatment, as they fear the consequences of a positive result. This can lead to delayed diagnosis and treatment, potentially impacting their health and well-being.
- Mental Health Impacts: The constant fear of stigma, discrimination, and legal repercussions associated with HIV can lead to anxiety, depression, and other mental health issues. This can further complicate the lives of individuals living with HIV, making it difficult to manage their condition and lead fulfilling lives.
Impact on Communities
HIV laws can also have significant consequences for communities, particularly those most affected by the epidemic. These laws can hinder efforts to prevent HIV transmission, reduce stigma, and promote access to healthcare.
- Barriers to HIV Prevention: Laws that criminalize certain behaviors associated with HIV transmission, such as sex work or drug use, can discourage individuals from seeking HIV prevention services or engaging in safer sex practices. This can lead to an increase in HIV transmission rates.
- Stigma and Discrimination: Laws that stigmatize and criminalize HIV-related behaviors can contribute to a climate of fear and discrimination, making it difficult for communities to access services and support. This can lead to increased isolation, marginalization, and vulnerability to HIV infection.
- Public Health Impacts: Laws that restrict access to HIV services, such as needle exchange programs or harm reduction initiatives, can have a detrimental impact on public health outcomes. These programs are essential for reducing HIV transmission and providing access to healthcare for vulnerable populations.
Epilogue

The story of HIV laws is a testament to the ongoing struggle to balance public health concerns with individual rights and freedoms. As new treatments and prevention strategies emerge, the legal landscape continues to evolve, prompting a reevaluation of existing laws and a search for more effective and equitable solutions. This journey through the history of HIV laws serves as a reminder of the profound impact of this epidemic, the importance of understanding the complex interplay of law and public health, and the ongoing need for compassion, empathy, and a commitment to human dignity in the face of a global health crisis.
FAQ Explained
What were the first HIV laws created?
The first HIV laws were primarily focused on public health measures, such as mandatory testing and contact tracing, and often included provisions for isolation and quarantine. These laws were often enacted in response to public fear and misunderstanding about the virus.
How have HIV laws changed over time?
Over time, HIV laws have evolved to incorporate a greater emphasis on human rights and individual freedoms. This shift has been driven by a growing understanding of the virus, advancements in treatment, and advocacy efforts by people living with HIV. More recent laws focus on reducing stigma, promoting testing and treatment, and protecting the rights of people living with HIV.
What are the current challenges surrounding HIV laws?
Current challenges include balancing public health concerns with individual rights, addressing stigma and discrimination, and ensuring access to treatment and prevention services for all. There are also ongoing debates about the criminalization of HIV exposure and the role of law in promoting harm reduction strategies.